Sign up for our newsletter, to get updates regarding the Call for Paper, Papers & Research.
Assessment of the Impact of Health Maintenance Organizations on Access, Utilization and Quality of Service among National Health Insurance Authority Enrollees in Kano, Kano State Nigeria.
- Gidado Yusuf
- Mustapha Muktar
- Amitabye Luximon-Ramma
- 1386-1400
- Apr 22, 2023
- Public Health
Assessment of the Impact of Health Maintenance Organizations on Access, Utilization and Quality of Service among National Health Insurance Authority Enrollees in Kano, Kano State Nigeria.
Gidado Yusuf 1*, Mustapha Muktar2, Amitabye Luximon-Ramma3
1School of Public Health, Texila American University, Guyana
2Dept of Health Economics, Bayero University, Kano State, Nigeria
3School of Health Science, University of Technology, Mauritius, Mauritius
*Corresponding Author
Received: 18 February 2023; Accepted: 23 February 2023; Published: 22 April 2023
ABSTRACT
Efforts by government in Nigeria in the past to provide effective ways of accessing quality and affordable healthcare service has always been contentious with high cost of health care service delivery. The ineffective management of health care funds over the years was observed as key contributor to the rising cost of healthcare services. The need for the establishment of health maintenance organizations (HMOs) whose responsibility as purchasers, was to manage health care services with health facilities providers under the National Health Insurance Authority Scheme (NHIA). However, this research seeks to assess the impact of healthcare purchasers in Kano state Nigeria, as regards knowledge, utilization and satisfaction of enrollees, whose healthcare services they managed. The study utilized analysis of enrollees, HMOs and desk officers under the scheme. Quantitative and qualitative methods using interviewer administered questionnaire and Key stakeholders’ interview were employed. Data were recorded in Microsoft Excel 2010 and analysed using SPSS version 23.0. NVIVO version 12 with verbatim transcription was used for thematic analysis of qualitative data. Chi-square was also used to test degree of association and logistic regression utilised to predict factors for the determinants. Results were presented as tables and charts. Statistical significance p-value <0.05 at confidence level of 95% was considered significant. Thus, analysis of the general demographic outcomes showed a significant association between HMOs and enrollees’ level of knowledge, utilization and satisfaction (p<0.05). Conversely, analysis of federal, state and private run facilities separately, revealed varying outcome as regards the three determinants, with the state-run hospitals mostly affected in terms of enrollee’s outcome.
Keywords: Desk officers, Health Maintenance Organizations, knowledge, National Health Insurance Authority, Satisfaction, utilization.
INTRODUCTION
The National Health Insurance Authority (NHIA) formerly known as the National health insurance scheme (NHIS) is a corporate body established under the NHIA ACT 2022 by the Federal Government of Nigeria to improve the health of all Nigerians at an affordable cost. It is a pre-payment plan where participants pay a fixed regular amount. The amount/funds are pooled, allowing the Health Maintenance Organizations (HMOs) to pay for those needing medical attention. It is primarily a risk pooling arrangement associated with the need to use and pay for health services rather than to be fully borne by the individual [1].
As such, it is the fiduciary duty of HMOs to effectively manage health care funds, provide quality care for the individuals whose health care they manage, and comply with all applicable laws and regulation governing the HMO scheme [2].
Health Maintenance Organizations (HMOs) are limited liability companies licensed by the National Health Insurance authority (NHIA) to facilitate the provision of healthcare benefits to contributors under the formal Sector Social Health Insurance Program. Existing arrangement makes HMOs to either be for-profit or not-for-profit private health insurance companies, or public entities [3]. Therefore, HMOs are constantly challenged with improving their internal controls to meet both regulatory and market demands from multiple stakeholders, while trying to maintain market share amidst competition from existing HMOs and new entrants into the managed care industry [4]. Sequentially in Nigeria, health Maintenance Organizations (HMOs) enrollment is growing substantially and Patient’s satisfaction is a key judgment on the quality and outcome of healthcare delivery and the extent to which the patients feel that their needs and expectations are being met by the service provider [5].
However, in Nigeria, the growing effort by government to provide effective ways of accessing quality and affordable healthcare coverage to attain universal health coverage has been contentious. The cost of health care delivery in Nigeria is high just like other developing country and this poses a serious threat to the country’s health care outcome as well as its health care system. The ineffective management of the government’s health care funds over the years was observed as key contributor to the rising cost of healthcare services. Nigeria is estimate to have a population of over 200 million people, the largest in Africa, among the West African countries [6]. It has the second highest density of physicians but still very low compared to the actual need for such a populous nation [7]. Government expenditure on health is considerably slimmer than what comes from private contributions. About 3.9 percent of Nigeria’s GDP is invested in the health sector, considerably below the average spending on healthcare among OECD countries [6] and Nigerians usually have to pay for medicine out of their own pocket. Often, the medicines are expensive and difficult to afford. In 2019, on average, health care made up six percent of Nigerian household spending, with higher figures in rural areas than in urban zones [8].
Also, on average, about 4% of households are estimated to spend more than half of their total household expenditures on health care and 12% of them are estimated to spend more than a quarter expenditure [9]. As health care costs are increasing faster than public revenues available for the health sector, economic constraints appear to have limited the amount of funds required to ensure universal coverage of necessary health interventions. The specific business problem is that, HMO leaders have also showed to lack internal control strategies to improve operational efficiencies, reduce health care costs, and improve quality of care for the individuals whose healthcare they manage [10]. As of 2018, about 97 percent of people surveyed in Nigeria did not have any health insurance. People with a health insurance mainly had an employer-based coverage and privately purchased insurances were notably uncommon. In total, only about three percent of individuals had a health insurance [8].
PROBLEM STATEMENT
Access and utilization of HMOs services resulting from medical intervention and qualitative healthcare services in various spheres of healthcare provision in Nigeria via the need for people to directly seek proper health care services has over the year account for serious health implication ranging from incomplete or sub-utilization of these services provided by HMOs and the attendant consequence on universal health coverage.
The considerable product differentiation and consequent risk selection by private insurers promote inefficiencies resulting from ineffective regulatory institutions and mandates to guide their behaviors towards attainment of public health goals and to identify and control undesirable business practices [11].Studies over the years have shown that access and utilization of public healthcare programs like NHIS in Nigeria is considerably low. Skepticism and lack of mutual trust of the public on government policies/programs culminating to cumbersome system, poor healthcare regulations, ineffective monitory and evaluation system has given rooms for fraud/corruption in the Health Maintenance Organization (HMO) operations [12]. The quality of healthcare service delivery under the existing health maintenance organizations (HMOs) in Nigeria has been a major concern to enrollees who have contested the value received from their respective HMO accredited hospitals under the program.
Findings revealed that HMO accredited hospitals have not ensured adequate access of enrollees to healthcare services, their responsiveness to enrollees’ healthcare requests have not been impressive, and quality of healthcare services to enrollees have also not been excellent. Study showed that, the performance of the HMOs in the area of healthcare service delivery is not world class when it comes to access, responsiveness, and quality of service delivery [13].
However, this study seeks to assess the impact of HMOs on access and quality of service on enrollees under the national health insurance scheme in Kano state, Nigeria. Thus, the study tends to amongst other things assess level of knowledge, utilization and satisfaction of enrolee of HMOs and contributory healthcare management agency as regards the national healthcare in selected health facilities in Kano State with a view to explore strategies HMOs used to improve operational efficiencies in order to provide quality care services for enrolees whose health care they managed.
Nonetheless, the study tends to bring to fore the role of purchasers of health care policies as regards their ability and capability of providing effective and efficient healthcare services as well as its impact on access to universal health coverage.
MATERIALS AND METHODS
A mixed study approach method was employed [14] That is, the quantitative study preceding the qualitative study (interview) of key stakeholders. This study method consisting of both qualitative and quantitative methods were used, such that most information is generated from the dominant study (quantitative), precedes the qualitative study based on that fact that, most variables of interest were generated from it and subsequently analyzed [ 15,16].
Study Area
Kano state is located in North Western region of Nigeria. Kano city which serves as the state capital, is the commercial nerve centre of Kano state and evitable the biggest in northern Nigeria and often referred to as the ‘centre of commerce’. According to the federal Republic of Nigeria official gazette 2009, the national population census provisional results of 2006 indicated that the population of Kano state was estimated to be about 9.4 million people and was considered the most populous state in the country [17]. The state has forty-four Local Government areas councils with an area of 20,479 square kilometres. Six of the local government councils are domiciled within the metropolis, while the remaining thirty-eight local government council areas are within rural areas and shares borders with Jigawa, Bauchi, katsina and Kaduna states. An estimated 1,346 health facilities are said to be located in the State according to the Kano state wide rapid health facilities assessment [18]. These include both public and private owned healthcare facilities.
Inclusion/Exclusion criteria
Enrollees at least 18 years or older and have used HMO for at least one year. HMO representatives responsibly for making operational decisions and have worked for at least 3 years with the organization. Health facilities focal person (desk officers) and have worked for at least 3 years with the health facilities.
Population and Sampling
The study Population includes enrollees under the national health insurance Authority in Kano state. The enrollees were proportionately selected amongst the three categories of health facilities (Federal, State and Private hospital) based on the number of patients registered under the NHIA scheme, as a more responsive approach because of their knowledge and understandings as adolescents and to explore their perceptions as regards the impact on services provided by their HMOs. Another study population were HMO regulatory officers and desk officers who were randomly selected from amongst the study groups with the NHIA scheme in Kano state, who are representatives as operating officers of their various organizations and have the responsibility for making operational decisions that aligned with the organization’s contractual and statutory regulatory requirements as well as oversight functions of the policies and procedures that guide the operations of their respective organizations.
Sample Size Determination
A cross sectional survey/study was carried and Purposive (Purposeful) sampling technique used to select the research participants. The Sample size formula for qualitative variable and quantities variable was employed to obtain the minimum sample size using the formula by Cochran [19].
n = Z2pq/e2
Where: n = the sample size, Z2 = Abscissa of the normal curve that cuts off an area α at the tails (1 – α equals the desired confidence level, e.g., 95%). It is Standard normal deviate corresponding to the confidence level of 95% for a tailed test = 1.96, e = Desired level of precision, which is 5% or 0.05, p = Estimated proportion of an attribute present in the population e.g., 59.7% (Proportion of utilization in a public facility [20], q = 1-p, Z= value of area under the normal curve (statistical table).
Using the formula above, the minimum sample size was ascertained thus; (1.96)2 X 0.597 X 0.407/ 0.05 X 0.05 = 0.933/0.0025 = 373
For non-response, an attrition rate of 10% was used. That is, 10% X 373 = 37. The likely Sample size to be used = 373 + 37= 410.
Sampling Technique:
Multi-stage sampling technique approach was carried out.
Stage 1: Some secondary and tertiary health facilities were sampled.
Stage 2: Proportional technique to determine the number of health facilities.
Stage 3: Proportional technique to determine the number of enrolees.
Stage4: Systematic random technique and semi-structured interview to identify/select HMO representatives and health facilities desk officers.
Data collection
A series of activities aimed at gathering and measuring suitable information to answer emerging questions were considered vital to the research. Thus, data collection process for both quantitative and qualitative study was employed [21]. Questionnaire enumerating determinants such as, enrolee’s demographic data, key research domains vis-a-vis, knowledge, utilization and satisfaction, quality of services provided by health facilities as well general appraisal was administered via study/research assistants using pre-testing evaluation, collection of data, recording the information and resolve field issues. Also, face-to-face, semi-structured interviews and personal observations data collection methods for the purpose of this study as part of reviewing vital records via key indicators (KI) was used. Accordingly, collection of reliable, pertinent data was critical to the soundness or validity of the study’s outcome and if repeated can generate the same research findings [22].
Data Analysis
Data evaluated were recorded in Microsoft Excel 2010 and quantitative variables calculated using Frequency distributions and analysis carried out using SPSS version 23.0. Chi-square test was also used to test degree of association between dependent and independent variable while multivariate analysis was used to compare variables. Logistic regression was equally employed to predict factors. NVIVO version 12 with verbatim transcription was then used for thematic analysis of qualitative data especially for the Key indicator Interview [23]. Statistical significance at p-value <0.05 at a confidence level of 95% was considered significant.
The reliability of this research for both quantitative and qualitative data collection was based on neutrality that generates consistent results and outcome to ensured conformability of all data collected and analysis of actual interpretation of participants’ views [24]. The concern of the study was demonstrated by intra-coder to establish the study’s reliability [25] and also replication of the findings, accuracy and the mitigation of error and bias [26] as well as review of the recordings of each interview several times before transcribing.
RESULTS
400 participants were selected for the study and data used as predictors of the impact of HMOs on Knowledge, utilization and satisfaction of services among NHIA enrollees in study area. All factors with a p-value of <0.05 were further subjected to multivariate analysis to identify the predictors of the impact of HMOs on knowledge, utilization and satisfaction of quality services among NHIS enrollees and to adjust for confounding variables as shown.
Table 1. Logistic Regression for predictors of Enrollees Knowledge on HMOs operations
| B | S.E. | Wald | Df | Sig. | Exp(B) | ||
| Age (<38 years) | -1.441 | .357 | 16.246 | 1 | .000 | .237 | |
| Gender (Male) | 1.156 | .307 | 14.131 | 1 | .000 | 3.177 | |
| Marital Status (Married) | .622 | .646 | .927 | 1 | .336 | 1.862 | |
| Number of Dependents Registered Under NHIS (Spouse only) | 18.640 | 4 | .001 | ||||
| Spouse & one child | .145 | .713 | .041 | 1 | .839 | 1.156 | |
| Spouse & two children | -.067 | .657 | .010 | 1 | .919 | .935 | |
| Spouse & three children | .569 | .705 | .651 | 1 | .420 | 1.766 | |
| Spouse & four children | 1.695 | .651 | 6.768 | 1 | .009 | 5.445 | |
| *Occupation (Civil servants) | 1.841 | .468 | 15.448 | 1 | .000 | 6.304 | |
| Monthly Income (<N65000) | -.993 | .312 | 10.152 | 1 | .001 | .370 | |
| *Source Of Information (HMO Canvassers) | 1.627 | .387 | 17.668 | 1 | .000 | 5.089 | |
| Constant | -2.702 | .738 | 13.427 | 1 | .000 | .067 | |
a. Variable(s) entered on step 1: Age -COLLAPSE, 2. Gender, Marital Status- COLLAPSE, 3.No. of dependents Registered Under NHIA, 4.Occupation -COLLASPE, 5.Monthly Income, Source of 6.Information -COLLAPSE.
*Statistically significant: (p<0.05)
*Non civil servants: Company workers, Bankers, Corp members, Artisans, Farmers
*Non-HMO Canvassers: Friends/Colleagues, Radio/Television, Newspapers, Workshops/Seminars, Internet.
The logistic regression shows that age, gender, number of dependents registered, monthly income and source of information have significant relationship with the level of knowledge, while marital status have no significant relation with level of knowledge. The study further showed the various variations as regards age, gender, number of dependent registered, occupation, income and sources of information as it affects the enrollee’s level of knowledge of HMOs operations.
Table 2. General Level of Knowledge of Enrollees of HMOs healthcare scheme
| Variables | Frequency (n=400) | Percentage |
| Level of Knowledge | ||
| Good Knowledge | 317 | 79 |
| Poor Knowledge | 83 | 21 |
| Total | 400 | 100 |
Source: Questionnaire 2022: HMO=Health Maintenance organization, n=400
The table shows that most (79%) of the respondents have good knowledge of HMO operations, while 21% have poor or inadequate knowledge.
Table 3. Logistic Regression for predictors of Enrollees utilization of services provided by HMOs
| B | S.E. | Wald | Df | Sig. | Exp(B) | ||
| Age (< 38 years) | 1.019 | .241 | 17.932 | 1 | .000 | 2.769 | |
| *Education (Degree) | .379 | .249 | 2.321 | 1 | .128 | 1.461 | |
| *Occupation (Civil servant) | -1.132 | .478 | 5.616 | 1 | .018 | .322 | |
| *Source Of Information (HMO Canvassers) | 1.436 | .294 | 23.843 | 1 | .000 | 4.203 | |
| Constant | -2.439 | .293 | 69.350 | 1 | .000 | .087 | |
a. Variable(s) entered on step 1: Age _COLLAPSE, Education-_COLLAPSE, Occupation-_COLLASPE, Source of Information-_COLLAPSE.
*Statistically significant: (p<0.05)
*Non-Degrees: Primary, Secondary, Diploma, Professional certificate, Islamic Education
*Non civil servants: Company workers, Bankers, Corp members, Artisans, Farmers
*Non-HMO Canvassers: Friends/Colleagues, Radio/Television, Newspapers, Workshops/Seminars, Internet.
The regression shows that age, occupation and source of information are significantly associated with level of utilization (p<0.05) of services provided by HMO, while educational qualification does not have significant relation with utilization. The study further revealed that those aged more than 38 years were almost 3 times poor in utilizing the scheme than those aged less than 38 years. This is also true for non-civil servants compared to civil servants. Enrollees from the study who get information from other sources other than through the HMO canvassers were 4 times observed to have poor utilization.
Table 4 General Level of Enrollees Utilization of services provided by health facilities under the HMOs
| Variables | Frequency (n=400) | Percentage |
| Level of Utilization | ||
| Good | 282 | 70.5 |
| Poor | 118 | 29.5 |
| Total | 400 | 100.0 |
Source: Questionnaire 2022: HMO =Health Maintenance organization, n=400
The table 4 shows the general Level of Utilization of services provided by health facilities under the HMOs. The overall outcome as regards the general level of utilization of services provided by the health facilities patronized by the respective HMOs showed that, the level of utilization of 70.5 % of respondents was good.
Table 5. Logistic Regression for predictors of Enrollees level of satisfaction with HMOs services in the hospital/clinics
| B | S.E. | Wald | Df | Sig. | Exp(B) | ||
| Age (< 38 years) | .747 | .227 | 10.787 | 1 | .001 | 2.111 | |
| *Education (Degree) | .403 | .237 | 2.891 | 1 | .089 | 1.497 | |
| *Source Of Information (HMO Canvassers) | 1.267 | .268 | 22.269 | 1 | .000 | 3.550 | |
| Constant | -2.112 | .261 | 65.298 | 1 | .000 | .121 | |
a. Variable(s) entered on step 1: Age_ COLLAPSE, Education_ COLLAPSE, Source of Information_ COLLAPSE.
*Non-Degrees: Primary, Secondary, Diploma, Professional certificate, Islamic Education
*Non-HMO Canvassers: Friends/Colleagues, Radio/Television, Newspapers, Workshops/Seminars, Internet
The logistic regression shows that, age and source of information are significantly related with level of satisfaction of services provided by HMO while educational qualification does not have significant relation with satisfaction The analysis further revealed that those aged more than 38 years are 2 times more likely to have dissatisfaction than those aged less than 38 years, those who get information from non-HMO canvassers are 3 and half times less satisfied.
Table 6: General Level of Satisfaction of Enrollees with the services in hospitals/clinics
| Level of Satisfied | Frequency (n=400) | Percentage |
| Level of Satisfaction | ||
| Satisfied | 270 | 67.5 |
| Dissatisfied | 130 | 32.5 |
| Total | 400 | 100.0 |
Source: Questionnaire 2022
The table 6 shows that the respondents were satisfied with the general Level of services of the health facilities (hospitals/clinics). The general level of satisfaction with services at the various health facilities from the study showed that, 67.5% of the respondents were satisfied, while 32.5% were dissatisfied.
Results of enrollees in Federal, State & Private run health facilities analyzed separately
Selected respondents (400 enrollees) were approached and consented to participate in the study giving a response rate of 100%. This second study below showed the findings of the health facilities run under the federal government, the state government and those run under private hospitals where the enrollees access service under their respective HMOs that managed them.
Data collected for enrollees in these three categories of health facilities were analyzed separately. The idea was to ascertain the level of service provided by the HMOs/Contributory health care management agency and how they differ in these 3 sectors. This was to give the research works an in-depth understanding as to whether services rendered/provided by the respective HMOs to enrollees in these three categories differs or not, or whether there are priorities giving to a particular category as regards services they provide to the enrollees. Thus, the whole idea was predicated on the fact that, from the general data collected, there were varying findings that showed some correlated differences in the results (respondents’ feedbacks) as regards services provided at these three categories of health facilities.
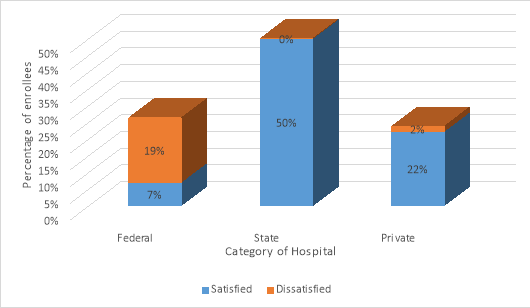
Fig1: Level of knowledge of HMOs by enrollees attending Federal, State and Private Hospitals
The chat demonstrates the level of knowledge of activities by the enrollees. Results showed that, all enrollees attending states facilities have good knowledge of their health management purchasers followed by those attending private hospitals. However, those in federal hospital seems to have a rather poor knowledge of their HMO’s activities.
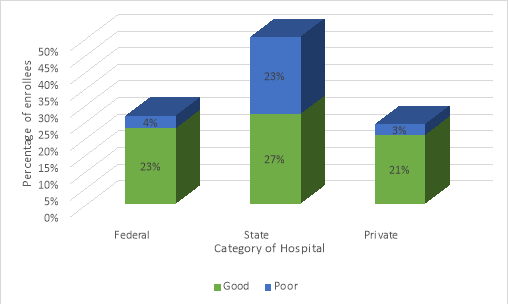
Fig2: Level of utilization of services as subscribed by the enrollees in Federal hospital, State hospital and Private Hospitals
Results shows the level of utilization as subscribed by enrollees. It revealed that, all the enrollees attending the three categories of health facilities shows profound utilization of their healthcare policies. However, enrollees under state run health contributory agency show to a rather more significant level of poor utilization.
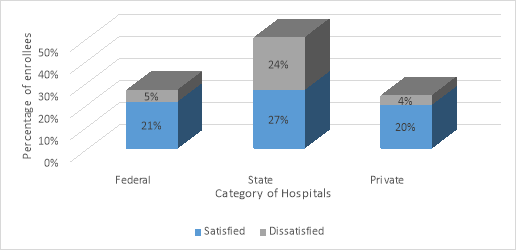
Fig3: General level of satisfaction by the enrollees attending Federal, State and Private Hospitals.
The results show the general level of satisfaction of enrollees in state run hospitals with varying perception. Though, there were significant level of satisfaction by enrollees in the state-run hospitals, they also seem to be more dissatisfied on their view about their healthcare services they enjoyed under their agency.
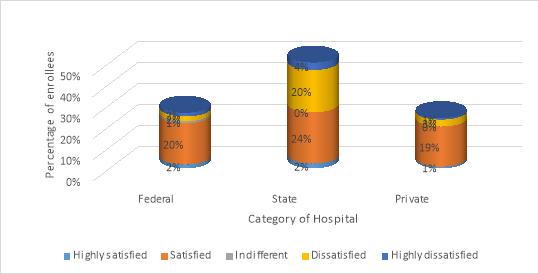
Fig4: Level of satisfaction of monitoring activities of the respective healthcare purchasers
The result above demonstrates the level of satisfaction of monitoring activities of the respective healthcare purchasers. Enrollees attending state hospitals showed a significant level of satisfaction with their health management monitoring of services in their respective hospitals compare to those of federal and private. Conversely, majority of enrollees attending state run hospitals showed more significantly dissatisfaction approval with the monitoring activities of their health facilities compared to the federal and state run.
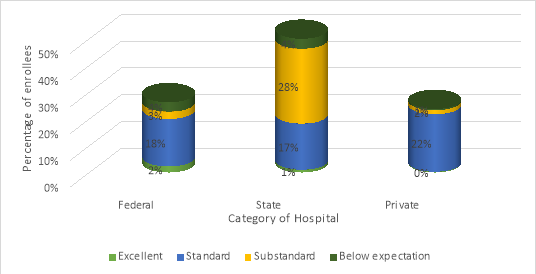
Fig5: General assessment of HMOs capacity
The results showed the general assessment of the capabilities in meeting contractual obligations of HMOs/Health contributory management agency to the enrollees. This result demonstrated that, the capacity of the state-run agency was the least in terms of meeting the enrollees’ expectations/obligations with respect to all the indicators as shown above.
Testing of Hypotheses
H01: There is no significant difference in the level of knowledge of enrollees of HMOs as regards the national healthcare insurance policy.
The chi-square value of H01 is 136.890 has a p-value <0.001, we therefore reject the first null hypothesis and conclude that there was significant relationship between the enrollee’s knowledge of the respective services managed by their HMOs.
H02: There is no significance relationship between the patronage and rate of utilization of services provided by HMOs to enrollees in Kano state.
The chi-square value of H02 is 66.257 has a p-value <0.001, we therefore reject the second null hypothesis and conclude that the level of utilization was significant high under the period of study, which indicated high level of utilization has a significant association with HMOs operations.
H03: There is no significant difference in the level of satisfaction of Services provided by health facilities managed by HMOs on Enrollees.
The chi-square value of H03 is 49.000 has a p-value <0.001, we therefore reject the third null hypothesis and conclude that majority of the respondents were satisfied with the general level of the services in hospitals/clinics.
Thematic analysis of key informant interviews of Representatives of Health Maintenance organization and Hospital Desk Officers on access, utilization and quality of service among national health insurance authority enrolees.
4 HMO representatives and 3 Hospital Desk officers were selected. The purpose of this qualitative study was to explore and access the organisational strategies of HMOs and hospital desk officer in terms of operational efficiencies in consonant with established guidelines and policies of the NHIA scheme. A semi structured interviews with four health maintenance organization /contributory healthcare management agency personnel and three desk officer each selected from the federal, state and private run health facilities operating in Kano. Data using transcribed interview were audio recorded, coded and then imported into NVivo12 software for thematic analysis. Overarching research questions and analysis were enumerated. Consequently, the impact of the HMOs internal control strategies of HMOs in meeting the health were evaluated. The analysis revealed varying degree of short comings on the part of HMOs and contributory health care management agency in meeting contractual agreement in terms of prompt remittance of capitation fee to the hospitals and lack of effective supervision amongst others. This was observed to have some implication in enrolee’s access to drugs and other secondary services. Equally, lack of adequate strategies and manpower to effectively monitor patient’s needs was observed to have also contributed.
DISCUSSION
The operations of health maintenance organisations or various health contributory management schemes over the years have remain contentious with regards their services as well as adherence to lay down rules and policy reforms for improving health care services in Nigeria. This has become necessary because efforts geared towards achieving universal health coverage as well as progressive evidence is considered necessary for financing policy reforms [27].
Accordingly, the quantitative aspect of the study assesses the impact of Health Maintenance organizations on access to quality health care service among National health insurance authority enrollees as regards, knowledge, willingness to utilize services and satisfaction with the quality of healthcare services provided by selected hospital facilities registered under HMOs in Kano State, Nigeria. Equally, the qualitative study (stakeholders’ interview) and thematic analysis was carried out to elucidate operational aspects of HMOs and desk officers of selected hospitals under the study jurisdiction. To this end, the results in the research provide some degree of’ insights of how these operations impacts on healthcare delivery with a number of key identified issues. Consequently, the outcomes of this study showed that, HMO performance in Kano state healthcare service delivery sector has varying scores. However, the logistic regression from the study in table 1 shows that age, gender, number of dependents registered, monthly income and source of information have significant relationship with the level of knowledge, while marital status have no significant relation with level of knowledge. On the whole, the general level of knowledge of enrolees about their respective HMOs operations showed that, most (79%) of the respondents have good knowledge of HMO activities, while 20% have poor or inadequate knowledge of HMOs activities. This study also brings to fore similarity with work of [28] which, reported high awareness (86%) among enrolled participants under similarly healthcare scheme.
Also, on the willingness of patients to utilize available services at the health facilities where they access services, the logistic regression in Table 3 shows that, age, occupation and source of information are significantly related with level of utilization of services provided by HMO while educational qualification does not have significant relation with utilization. However, the general level of Utilization of services by enrollees in the health facilities showed that, the level of utilization was significantly high, about 70.5%. However, the high level of utilization of services by enrollees would have probably been as a result that, enrollees do not have to directly spend out of their pockets before accessing healthcare services in hospitals. This is in agreement with similar study by Patel et al [29] on the Post Utilization Survey of Rashtriya Swasthya Bima Yojana in Shala and Kangra Districts in Himachal Pradesh (RSBY) about beneficiaries’ utilization of service not directly paid for. It could also be explained likely from improved services of registered hospitals under the scheme in terms of personnel and equipment in recent years, though there was no comprehensive evidence to show that this high rate of utilization is synonymous to quality of service provided to enrollees from the study.
Accordingly, the attitude of healthcare provider while providing services influences enrollees’ level of satisfaction [30].Similarly, in this study, there was unanimous opinion among the enrollees, with majority of the respondents revealing that, the overall reception of staff towards them were encouraging.
The logistic regression in Table 5 shows that age and source of information are significantly related with level of satisfaction of services provided by HMOs, while educational qualification does not have significant relation with satisfaction. However, results showed that, majority of the respondents expressed general level of Satisfaction with services in the hospitals/clinics with 67.5% of the respondents were satisfied while 32.5% were dissatisfied. This result also shows similarity with studies in Calabar, Ife and Nnewi in Nigeria with respect to enrollee’s satisfaction with provision of services under the NHIA scheme [31, 32, and 33].
Conversely, thematic analysis of key informant interview of representative of HMO and hospital desk officer, revealed varying degree of short comings on the part of HMOs and contributory health care management agency in meeting contractual obligations in terms of prompt remittance of capitation fee to the hospitals, lack of effective strategy and inadequate manpower. These were observed to have some implications on enrolee’s access to secondary services.
RECOMMENDATIONS
In view of the foregoing, the following recommendations would go a long way in solving the most sticking outcomes needed, if only involvement of providers as well as purchasers of healthcare services at both the federal and state level would add value to ensure effective implementation of the national health insurance scheme to meet the universal healthcare coverage for Nigerians.
- The NHIA should expand their monitoring and supervisory capacity to look at the state run contributory health care management agencies under the insurance scheme as well as accredited facilities’ mode of operations. Some facilities with limited capacity go into agreement with HMOs for some services they are incapable of providing.
- The Kano state contributory healthcare management agency to involve private run HMOs in their operations rather than managing it themselves to ensures efficiency and proper implementations of standard policies and procedures of the scheme.
- Health facilities managers should ensure proper documentation of bills and claims to ensure hitch free reconciliation processes to avoid claims and counter claims which often time resulted in loss of funds and delay in service provision to enrolees.
CONCLUSION
Results from the general quantitative study (i.e., Data of all enrollees analyzed together) both agreed that, there was some level of improvement on the three key research domains as regards knowledge, utilization and satisfaction with respect to the roles of HMOs/contributory health care management agency in the state. However, analysis carried out separately with the three categories of health facilities (federal, state and private run hospitals) revealed that, enrollees in state-run hospitals managed by the State health contributory agency were mostly affected in terms of meeting their health care needs under the state healthcare insurance scheme. Conversely, responses of HMO managers in the qualitative study did not totally support the argument from the perspective of desk officer’s submissions. The study however revealed that, HMOs as well as the state-run contributory heath management agency were not as effective and efficient in meeting their obligations.
FUTURE RESEARCH
- There is a need for in-depth research about the role of state-run insurance Agencies to ascertain their level of capacity in meeting healthcare need of their employees in line with the NHIA expectations.
- The need for proper Evaluation of providers (hospitals) capabilities in providing secondary and tertiary services under the NHIA scheme.
- Monitoring and evaluation by NHIA to identify best practices of providers and purchasers of the scheme to ensure consistency and eliminate fraudulent practices.
ACKNOWLEDGMENTS
I do acknowledge all the respondents (Enrollees, HMOs officers and hospital desk officers) who took time to participate in this study.
CONFLICTS OF INTEREST
The author declares no conflicts of interest.
REFERENCE
- Kutzin J., 2001, A descriptive framework for country-level analysis of health care financing arrangements. Health policy (Amsterdam, Netherlands), 56(3)171–204. https://doi.org/10.1016/s0168-8510(00)00149-4.
- Pozgar, G., 2016, Legal and Ethical Issues for Health Professionals (4th ed.). Burlington, MA: Jones & Bartlett Learning. Date of Access: 23/6/2021, https://samples.jblearning.com/9781284036794/9781284069761_FMxx_Cropped.pdf
- Odeyemi, I. A., and Nixon, J., 2013, Assessing equity in health care through the national health insurance schemes of Nigeria and Ghana: a review-based comparative analysis. International journal for equity in health, 12, Article number 9. https://doi.org/10.1186/1475-9276-12-9.
- Chen, A and Goldman, D., 2016, Health care spending: Historical trends and new directions. Annual Review of Economics, 8, 291-319. doi:10.1146/annureveconomics-080315-015317.
- Zohrevandi, B., & Tajik, H., 2014. A Survey of Patients’ Satisfaction in Emergency Department of Rasht Poursina Hospital. Emergency (Tehran, Iran), 2(4), 162–165.
- Doris, D.S., 2022, Health in Nigeria -statistics and facts. Date of Access: 20/11/22, https: //www.statista. com.
- Lars, K., 2022, Density of physicians in west Africa 2020 by country. Date of Access: 20/11/22, https://www.statista.com/statistics/1122671/density-of-medical-doctors-in-west-africa-by-country/
- V., 2021, Government’s healthcare expenditure in Nigeria 2019-2021. Date of Access: 2/7/21,https:// www. statista.com/aboutus/our-research-commitment/ 1914/ simona-varrella.
- Uzochukwu, B. S., Ughasoro, M. D., Etiaba, E., Okwuosa, C., Envuladu, E., and Onwujekwe, O. E., 2015, Health care financing in Nigeria: Implications for achieving universal health coverage. Nigerian journal of clinical practice, 18(4), 437–444. https://doi.org/10.4103/1119-3077.154196
- Elizabeth, E.D., 2020, A Health Care Management Organization’s Internal Controls Strategy for Managed Care” Walden Dissertations and Doctoral Studies. 9345. https://scholarworks.waldenu.edu/dissertations/9345
- Onoka, CA., Kara H., Anne M., 2016, Growth of health maintenance organization in Nigeria and the potential for a role in promoting universal health coverage. doi:10.1016/jsocscimed.2016.06.018.
- Adeoye TO., Indabawa S., Abdulsalam F., Oboh T., 2007., Report of service utilization survey among NHIS accredited primary healthcare providers-Katsina, Kano and Jigawa state.
- Akinbode, J O., Eniola, AS., and Muideen, O A., 2019, Appraisal of Health Maintenance Organizations ’Performances in the Nigerian Healthcare Service Sector. Journal of healthcare Engineering, https://doi.org/10.1155/2019/6820609.
- Wao, H and Onwuegbuzie, A.J., 2011, A Mixed Research Investigation of Factors Related to Time to the Doctorate in Education. International Journal of Doctoral Studies, 6, 115-134.
- Akinbode, J O., Eniola, AS., and Muideen, O A., 2019, Appraisal of Health Maintenance Organizations ’Performances in the Nigerian Healthcare Service Sector. Journal of healthcare Engineering, https://doi.org/10.1155/2019/6820609
- Molina, A.J.F., and Fetters, M.D., 2018, Future Special Issues at the Journal of Mixed Methods Research. Journal of Mixed Methods Research,12(4),369–370, https://doi.org/10.1177/1558689818800897
- Sánchez, H.A., and Alcón, S.E., 2011, Pragmatic gains in the study abroad context: Learners’ experiences and recognition of pragmatic routines, Journal of Pragmatics, 146, 54-71.
- Federal Republic of Nigeria., 2009, National Population Commission Official Gazette. National Population Commission, Abuja. 2 Vol.96.
- Kano State Ministry of Health, Kano SACA, IHVN and FHI 360., 2013, Kano State-wide Rapid Health Facility Assessment, Nigeria: Kano State Ministry of Health, Kano State Agency for the Control of AIDS, IHVN and FHI 360.
- James, E.B., 2001, Organizational research: Determining appropriate sample size in survey research.
- Daramola, O.E., Adesina, C.T., Abu, J.M., and Akande, T.M., 2019, Health Services Utilization Patterns among Enrollees of the National Health Insurance Scheme at a Tertiary Health Facility in Federal Capital Territory (FCT) – Abuja, Nigeria.
- Elo, S., Kaariainen, M., Kanste, O., Polkki, T., Utriainen, K., and Kyngas, H., 2014, Qualitative content analysis: A focus on trustworthiness. Sage Open, 4(1), 1-10. doi:10.1177/2158244014522633.
- Saunders, M.N.K., and Rohon, C., 2014, There’s no madness in my method: Explaining how your coaching research findings are built on firm foundations. Coaching: An International Journal of Theory, Research and Practice, 7, 74-83. doi:10.1080/17521882.2014.889185
- Woods, M., Paulus, T., Atkins, D. P and Macklin, R., 2016, Advancing Qualitative Research Using Qualitative Data Analysis Software (QDAS)? Reviewing Potential Versus Practice in Published Studies using ATLAS.ti and NVivo, 1994–2013.Social Science Computer Review, 34(5),597–617, https://doi.org/10.1177/ 0894439 3155963 11
- Teusner, A., 2016, Insider research, validity issues, and the OHS professional: one person’s journey. International Journal of Social Research Methodology, 19, 85 – 96.
- Nelson, A.M., 2016, Methodology for examining attributes of African Americans in the Department of Defence Senior Executive Service Corp. Journal of Economic Development, Management, IT, Finance and Marketing, 8, 48-68.
- Anney, V., 2014, Ensuring the quality of the findings of qualitative research: Looking at trustworthiness criteria. Journal of Emerging Trends in Educational Research and Policy Studies, 5, 272-281.
- Lagarde, M and Palmer, N., 2011, The impact of user fees on access to health services in low- and middle-income countries. The Cochrane database of systematic reviews, (4), CD009094, https://doi.org/10.1002/14651858.CD009094.
- Mohammad, A., 2013.Evaluation Study of Rashtriya Swasthya Bima Yojana in Shala and Kangra Districts in Himachal Pradesh. Date of Access: 9/11/2022, http://www.rsby.gov. in/Documents.aspx?ID=14.
- Patel, J., Shah, J., Agarwal, M., Kedia, G., 2013, Post Utilization Survey of RSBY beneficiaries in civil hospital, Ahmedabad: A cross sectional study. International Journal of Medical Science and Public Health. 2(4):1109-12.
- Iliyasu, Z., Abubakar, I.S., Abubakar, S., Lawan, U.M.., and Gajida, A.U., 2010, Patients’ satisfaction with services obtained from Aminu kano teaching hospital, Kano, Northern Nigeria. Journal of Scientific Research, 11, 1.
- Apeloko, O.D., 2017, Health Insurance Scheme (NHIS) in Nigeria: An Empirical Survey. International Journal of Politics and Good Governance. (8):1–25.
- Ele, G.N., Ochu, U., Odili, V., Okechukwu, R., Ogbonna, B., 2016, Evaluation of the Benefits, Quality of Services and Challenges to the Nigerian National Health Insurance Scheme among Enrollees in a Tertiary Teaching Hospital in Southeast Nigeria. journal of Advance Medical Pharmaceutical Science. 10;9(3):1–11.
- Osuchukwu, N.C., Osonwa, K.O., Eko, J.E., Uwanede, C.C., Abeshi, S.E., Offiong, D.A., 2013, Evaluating the Impact of National Health Insurance Scheme on Health Care Consumers in Calabar Metropolis, Southern Nigeria. Int J Learning Develop. Vol 3(4):30-45.

