Sign up for our newsletter, to get updates regarding the Call for Paper, Papers & Research.
Phenomenology & Ethnography: Examining Hospital Cultures and the Lived Experiences of Patients Interacting with Healthcare Professionals
- Dr. Denise Gates-Mayweathers
- 64-88
- Feb 26, 2024
- Health Education
Phenomenology & Ethnography: Examining Hospital Cultures and
the Lived Experiences of Patients Interacting with
Healthcare Professionals
Dr. Denise Gates-Mayweathers
DOI: https://dx.doi.org/10.47772/IJRISS.2024.802005
Received: 08 January 2024; Revised: 22 January 2024; Accepted: 27 January 2024; Published: 26 February 2024
ABSTRACT
This exploratory ethnographic and phenomenological study examined hospital cultures, primarily emergency rooms, and the lived experiences of patients interacting with healthcare professionals in the United States. The salient themes that emerged from the thematic analysis of the narratives shared by a woman living with asthma in conjunction with the lived experiences articulated by five other patients coming to emergency rooms for stomach pain/pregnancy, arthritis/joint pain, leg injury, depression, etc., were: 1) Long wait times, 2) Poor and Unprofessional Attitude, 3) Neglect, 4) Feeling Rushed, 5) Having to Ask for Care, 6) Discrimination, and 7) Support from Hospital Patient Advocates and Other Patients. While the patients in this study endured marginalization and microaggressions, those challenges often were overcome with assistance from hospital patient advocates as well as other patients. Ultimately, patients in this study empowered themselves to achieve their healthcare goals.
INTRODUCTION
While health is always a priority for some people, COVID-19 probably has individuals around the globe reexamining their health and rethinking many of the daily decisions they make in order to sustain healthy lifestyles. As COVID-19 went into full swing, people everywhere went into crisis mode as societies tried to understand what was happening while attempting to adhere to shelter-in-place orders. The COVID-19 crisis sent some people into a panic, and individuals with preexisting conditions, such as asthma, emphysema, and heart disease, were especially concerned because COVID-19 tended to be more deadly for people who already were managing illnesses, according to Gupta et al., (2021).
COVID-19 certainly placed great stress on healthcare facilities, magnifying their existing problems. One salient challenge that emerged as a problem was prioritizing the demands for medical attention. Healthcare professionals were forced to determine how, with limited resources, to meet the demands of a society facing a health crisis. These circumstances resulted in some people not getting the care they wanted and deserved. When time and other resources were limited, healthcare professionals made tough business decisions, choices that historically placed some non-dominant racial groups at a disadvantage (Funk, 2022; Nix, 2023).
One group that historically has endured compromised healthcare was African Americans/Blacks (Duncan et al., 2022). “Black patients have experienced centuries of mistreatment and violence at the hands of the medical system, which has made the medical system untrustworthy” (2022, p. 520). Nix (2023) substantiated this claim as well. Banerjee and Sanyal (2012) also found that women were less trustful of doctors, compared to men, when it came to their care. Funk (2022) also echoed the sentiment that African Americans/Blacks were subjected to marginalization in healthcare systems.
Less access to quality medical care is the top reason Black Americans see contributing to generally worse health outcomes for Black people in the U.S. Large shares also see other factors as playing a role, including environmental quality problems in Black communities and hospitals and medical centers giving lower priority to the well-being of Black people…A majority [of African Americans] (56%) say they have had at least one of several negative experiences, including having to speak up to get the proper care and being treated with less respect than other patients (Funk, 2022).
Research by Funk (2022) revealed that African American/Black women more frequently than other groups had negative experiences with healthcare professionals. Studies revealed that African American/Black women: 1) Had to speak up to get help, 2) Believed pain was not taken seriously, 3) Felt rushed by healthcare professionals, 4) Felt like they were treated with less respect than other patients, 5) Felt that their quality of care was less than what other patients received, 6) Were judged due to weight, and 7) Found that health concerns were not taken seriously. However, they indicated that quality of care was better when African American/Black healthcare professionals treated them, which was consistent with research by Snyder et al., (2023). However, many healthcare facilities did not have much diversity among their personnel, resulting in African American/Black patients relying on cross-cultural communication with Caucasian/White healthcare professionals and other races for care.
The Centers for Disease Control and Prevention (2023) also suggested that African Americans/Blacks, as well as other traditionally disenfranchised groups, had experiences with healthcare systems that were less than stellar, suggesting that a more profound examination into the ways in which healthcare professionals have been socialized (Gates, 2009, 2023a; 2023b) into organizations that treat patients is warranted. Specifically speaking:
A growing body of research shows that centuries of racism in this country have had a profound and negative impact on communities of color. These conditions—often referred to as social determinants of health—are key drivers of health inequities within communities of color, placing those within these populations at greater risk for poor health outcomes (Centers for Disease Control and Prevention, 2023).
The systems that rendered certain social groups marginalized may have impeded the ability of some individuals to manage and recover from illnesses as well as their Caucasian/White counterparts recovered. Heredity, lifestyle choices, and other factors also influence the health of African Americans/Blacks, but clearly, people from non-dominant racial groups seem to experience disease and death more frequently than Caucasians/Whites, according to the Centers for Disease Control and Prevention (2023). People from non- dominant racial groups, such as African Americans/Blacks and Latinos, experience higher rates of illness and death than Caucasians/Whites, and asthma was among the many illnesses from which they died.
Rationale
Given the reliance of African Americans/Blacks, as well as other racial groups, on emergency rooms and other healthcare facilities for treatment, scholars and practitioners may benefit from enhancing their comprehension of how African Americans/Blacks experience healthcare. The health disparities within the United States have rendered African Americans/Blacks seeking healthcare marginalized, and it is imperative to address the matter. “To build a healthier America for all, we must confront the systems and policies that have resulted in the generational injustice that has given rise to racial and ethnic health inequities,” according to the Centers for Disease Control and Prevention (2023, p. 1).
This paper will discuss the dynamics between healthcare professionals and patients as these interactions have shaped the perceived quality of care from healthcare professionals. It is crucial to address the disparities in healthcare because people from non-dominant racial groups receive compromised care in many instances. Moreover, African Americans/Blacks are dying at a faster rate than their Caucasian/White counterparts, according to the Centers for Disease Control and Prevention, in part because the quality of care from healthcare professionals has been substandard.
Problem
According to the Centers for Disease Control and Prevention (2023), nearly 25 million Americans are living with asthma as of 2021. Of those 25 million people, about 14 million are women or girls, and over 4 million of the people with asthma in the United States are African American/Black. Moreover, more than 4.8 million physician office visits in the United States during 2019 were due to asthma, according to the Centers for Disease Control and Prevention (2023). Similarly, the National Center for Health Statistics (2023) reported that the number of visits to emergency rooms in the United States in 2021 for asthma as the primary diagnosis, excluding chronic obstructive asthma, was 939,000. Therefore, nearly one million emergency room visits and almost five million doctor visits were due to asthma (Center for Disease Control and Prevention, 2023; National Center for Health Statistics, 2023). Finally, a total of 3,517 people in the United States died of asthma in 2021 (Centers for Disease Control and Prevention, 2023), which suggests that more information about how healthcare professionals interact with asthma patients and treat asthma could help healthcare professionals enhance care.
With so many people experiencing asthma in the United States (Centers for Disease Control and Prevention, 2023), it might help to make sense of the lived experiences of an asthma patient as well as other patients, particularly individuals from traditionally marginalized groups. Relative to other studies, fewer studies tend to focus on how a woman of Native American and African descent experiences healthcare facilities. The need for more research in this area justifies an exploratory ethnographic and phenomenological study examining the interactions among healthcare professionals and patients. This topic is relevant today because past research has suggested that people from traditionally marginalized groups, such as women and African Americans/Blacks, do not enjoy the same quality of care as people who are Caucasian/White Americans (Fix et al., 2022; Funk, 2022). The present study illuminates the obstacles a particular woman encountered on her journey to combat asthma and encompasses a cursory view of the lived experiences of five other patients.
LITERATURE REVIEW
Research addressing the interaction between healthcare professionals and patients has covered a plethora of topics, and some of the salient themes that emerged from that research had to do with the length of wait times (Karaduman et al., 2023; Spechbach et al., 2019), attitude or professionalism (Karaduman et al., 2023; Ming et al., 2019), and discrimination (Alvarez et al., 2019; Bird et al., 2021; Haywood et al., 2014; John et al., 2021). The forthcoming paragraphs will address long wait times, poor attitudes, lack of professionalism, and discrimination within healthcare.
Long Wait Times
A primary concern regarding healthcare was long wait times (Acar, 2018; Karaduman et al., 2023). Patients were typically willing to wait an hour or two, but anything longer than that was deemed excessive (Spechbach et al., 2019). One population that tended to struggle with long wait times was people living with mental illness. Emergency room boarding of psychiatric patients is too long (Alakeson et al., 2010). Patients who need inpatient beds spend too much time waiting for care in the Emergency Department waiting room, hallways, and restrooms. Some leave healthcare facilities before treatment (Alakeson et al., 2010). Delivery systems that provide mental health support need to be enhanced to reduce emergency room stays and to prevent jail time as these individuals in distress re-enter communities where they end up getting arrested, or they become victims of suicide due to an ongoing lack of treatment. Community-based support, as well as reduced waiting times for appointments, can be helpful. Because emergency rooms can be noisy and stressful, sometimes the environment can exacerbate the mental episode (Alakeson et al., 2010). Long wait times can be problematic, and the stress of long wait times can be compounded by poor attitudes, which will be discussed next.
Poor Attitudes
Karaduman et al., (2023) said poor attitudes compromised perceived quality of care. In a study of approximately 1385 complaints, patients had concerns about healthcare professionals, primarily about poor attitudes and long wait times. Complaints filed in 2019 against doctors and other healthcare professionals were processed by a department overseeing patient rights in Turkey. In another study, Ming et al., (2019) reviewed complaints against nurses at a university-sponsored hospital in China. Results indicated that “uncompassionate attitudes, unprofessional communication, disrespect of patient rights, and unsatisfactory quality of nursing care” were the salient themes emerging from complaints. Poor attitudes and disrespectful conduct can undermine the perceived quality of care.
Discrimination
Discrimination in healthcare has been a problem for decades. In the infamous syphilis studies, which started in 1932, researchers convinced doctors not to treat African American/Black men for the disease, so they could study it (Nix, 2023). The doctors knew that penicillin could easily cure the disease, but they neglected to give it to the patients. Instead of medicine, the men were given aspirin and mineral water. As a result, many men died of syphilis, and others infected their loved ones with the disease. Some had children who were born with the illness. The disastrous outcomes could have been prevented if healthcare professionals and researchers had been more ethical. Nix (2023) explained:
Health workers monitored the men but were only given placebos such as aspirin and mineral supplements, even though penicillin became the recommended treatment for syphilis in 1947, some 15 years into the study. PHS researchers convinced local physicians in Macon County not to treat the participants, and instead, research was done at the Tuskegee Institute (p.1).
The Tuskegee studies, whereby African American/Black men were denied treatment so the disease could be studied, inspired a lack of trust in the healthcare system. Many African Americans became distrustful of healthcare professionals, the use of vaccinations, and the appropriateness of medication prescribed for them. This distrust, coupled with other anti-African American/Black rhetoric/actions from healthcare professionals, has compromised the care of many African Americans/Blacks (Nix, 2023).
Does this distrust of healthcare professionals have anything to do with why African Americans/Blacks and Latino Americans often do not have primary care physicians (Berthelot et al., (2020)? African Americans/Blacks and Hispanic Americans often did not have primary care physicians, and they tended to use emergency rooms for services they could have easily obtained with primary care physicians, according to Berthelot, Lang, and Messier (2020) as well as Shea et al., (1992). The patients in the study by Shea et al. (1992) were from New York, and they did not regularly check their blood pressure because they were not seeing their primary care physicians where it could be done. As a result, these patients ended up in emergency rooms with issues stemming from blood pressure problems. Sometimes, they were not taking their medication as prescribed (Shea et al., 1992). Today, patients can easily check their blood pressure at home or at their local pharmacies, but a low commitment to doing this may result in more emergency room visits. Alternatively, when patients discover problems with blood pressure, they go to emergency rooms, not their primary care providers, because it is often faster to go to emergency rooms. When patients discover that their blood pressure is too high, waiting weeks to see a primary care physician is not the most prudent approach to tackling the problem. Most patients want immediate care, which can most likely be found in an emergency room, not the small offices of primary care physicians who lack the adequate equipment to treat patients in crisis. While many patients may go to emergency rooms because they do not have primary care physicians, others elect to go to emergency rooms because that is the fastest way to see a doctor.
Primary care physicians often are more accessible than one might assume. Even impoverished people can get state insurance via Medicaid and locate a primary care physician unless they do not like their options. Not all healthcare professionals accept Medicaid, and some patients may not want to be partnered with the healthcare professionals from which they must choose. The distrust of primary care physicians could be one reason people do not have a personal doctor, or patients perceive that they cannot afford a doctor. Astronomical healthcare costs can preclude some people from accessing good doctors.
The prevalence of marginalization within the field of healthcare may spur some patients to rethink their healthcare choices, as Kyerematen et al. (2023) assert that anti-Black racism is prevalent in the field of medicine even today. Empathy and inquiry tended to be approaches healthcare professionals employed to address anti-racism. However, this was not enough. A more comprehensive approach to combatting racism in the healthcare industry is warranted. The authors recommend accountability and allyship to help eradicate racism. Anti-racism communication strategies need to be employed to promote equality for African American/Black patients. Promoting racial justice and health equity in treating African American/Black patients is vital to adequate care (Kyerematen et al., 2023).
Women also felt marginalized within healthcare systems, which may be part of the reason they were found to be less trustful of doctors relative to other patients. Banerjee and Sanyal (2012) found differences across genders in the perception of treatment from healthcare professionals with women being less trustful of doctors than men. Research also showed that doctors did more partnership building with male patients than they did with women (Banerjee & Sanyal, 2012). These researchers also suggested that “language and culture, alternative medicines, commercialization of medicine, and crowding at specialist and super- specialist clinics [were other] barriers to a good doctor-patient relationship” (Banerjee & Sanyal, 2012). Future research needs to determine if these findings are still prevalent today.
John, Curry, and Cunningham-Burley (2021) studied pregnant women, whom the authors classified as Black, Asian, and minority ethnic women. The findings were categorized as “communication, interactions with healthcare professionals, racism, and the pandemic effect.” While the pregnant women appreciated some aspects of their care, they noticed bias. They perceived that they were discriminated against based on their language and accents, and they also asserted that language barriers were the primary cause of miscommunication. The women perceived that once a woman’s accent was heard, she was not taken seriously. Cultural dissonance was a barrier to communication between pregnant women and healthcare providers.
The pregnant women welcomed respectful communication, continuity of care, empathy, and informed decision-making. Empathy was appreciated. However, when doctors hurry the women, they feel uncared for and unappreciated (John et al., 2021). When healthcare professionals were deemed indifferent toward patients, the women stated that they felt hurried, unheard, and uncared for, which negatively shaped perceptions about care (John et al., 2021, p. 4). John et al. (2021) asserted:
Institutional racism was highlighted as a significant issue in pregnancy care by most of the participants. Some of the participants expressed distrust in maternal healthcare due to their concerns that medical research and treatments are tailored for their White counterparts. Participants who had experienced institutional racism were also likely to perceive barriers to accessing healthcare compared with White women (p.5).
Overall, pregnant women were marginalized in healthcare systems and sought respectful interactions.
Negative differential treatment in healthcare has not always been about race or gender. In addition to race-based discrimination, patients living with Sickle Cell Disease felt discriminated against by healthcare providers due to their illness (Alvarez et al., 2019). The stigma of having certain illnesses can cause healthcare professionals to mistreat patients. Consequently, marginalization is exacerbated when people from non-dominant racial groups have a disease. Patients felt disenfranchised due to their illness and again because of the intersection of their race and gender. Ultimately, the health inequities and systematic differences were noted by patients. However, other research examined how healthcare professionals experienced the complaints (Glera, 2019), which will be addressed in the following section.
Managing Complaints
While much of the extant research has assessed patient complaints against healthcare professionals, other studies focus on how healthcare professionals experience those complaints. Glera (2019) said the complaints are stressful for healthcare professionals in London, and some healthcare professionals have taken their own lives as a result of complaints filed against them. Organizations need to comprehend the influence complaints have on the mental health of providers. As a result, complaint codes might be one way to help minimize the impact complaints have on doctors. Glera stated:
A serious complaint can take years to pass through the regulatory system, leaving the doctor stuck in a confusing matrix of fear, uncertainty, and anxiety. The complainant has a tried and tested framework that everyone involved—managers, clinicians, organizations—must follow. Those complained about have no similar framework. A serious complaint can take years to pass through the regulatory system.
Moreover, 70 percent of complaints against healthcare professionals in Iran were deemed unmerited, according to Alimohammadi et al., (2019). Therefore, healthcare organizations need systems in place to launch investigations prior to taking action against healthcare professionals, and disciplinary actions need to be deemed fair, according to Dyer (2023). Hospitals should also be cognizant that complaints against healthcare professionals can be stressful (Glerada, 2019) as doctors fear losing their jobs or having their medical licenses revoked. Workplace stress can be traumatizing and entice employees to contemplate leaving organizations (Gates, 2023b) or to determine how best to manage the stress (Gates, 2010; 2023b). While complaints against healthcare professionals can be stressful for doctors and other employees, these grievances do have some utility.
Patient complaints can be used as feedback to focus on improvements (Grandizio et al., 2022). They should not automatically be regarded negatively. Instead of seeing complaints as a personal attack on healthcare professionals, organizations can reframe complaints as patient input to make improvements (Grandizio et al., 2022). Patient-centered care requires healthcare professionals to understand the cultures and concerns of patients in order to provide optimal care. Perhaps healthcare professionals need to be socialized (Gates, 2009; 2023a; 2023b) to reframe complaints as feedback designed to help them remain patient-centered so they can enhance patient care.
Recent trends in healthcare regarding the quality of interactions between healthcare professionals and patients, as well as equal access to healthcare, warrant greater examination. Scholars and practitioners need a more in-depth analysis of these interactions, particularly given the prevalence of marginalization and microaggressions endured by patients from non-dominant racial groups. The prominence of racism within the healthcare industry suggests that a more profound focus on the communication between healthcare professionals and patients may help leaders devise plans to eradicate racism. This dynamic deserves more attention because many of the patients coming to hospitals and emergency rooms for treatment are from non- dominant racial groups, and they are not getting the quality of care they need. Organizations must identify the systems that engender marginalization in healthcare so they can create strategies to promote equality for all patients. Future research must analyze the perspectives of patients on communication practices by healthcare professionals that promote anti-racism (Duncan et al, 2022; Kyerematen et al., 2023). While past research has focused on the experiences of patients from various backgrounds, the present ethnographic and phenomenological study will explore the encounters of people from traditionally marginalized groups as they interact with healthcare professionals.
Research Questions
- How do patients experience healthcare professionals?
- How do patients from traditionally disenfranchised groups experience emergency room cultures?
- What tactics can patients in this study employ to combat marginalization within healthcare systems?
METHODS
The impetus for this study was an unusually long wait time in the emergency room to be treated for asthma at a hospital in the United States. Four women of African and/or Native American descent, one man of African descent, and one openly gay, Caucasian/White man all happened to be in the same hospital at the same time. They did not previously know each other, but they collectively complained about the long wait times in the emergency center. As the patients compared notes, those shared experiences prompted additional inquiry into hospital wait times and experiences in emergency rooms in general.
The author utilized ethnography and phenomenology as qualitative research methods to conduct an exploratory study examining the lived experiences of a woman from a non-dominant racial group as well as the hospital cultures in which the woman interacted with five other patients and various healthcare professionals (Creswell, 2013; 2015; Creswell et al., 2011; Creswell & Plano Clark, 2011; Levitt et al., 2018; Lindlof & Taylor, 2011). This approach to the present research was appropriate because eethnography started as an attempt to study and describe social actions within cultures; ethnographers sought to identify how people interacted within a given culture (Spradley, 1979, 1980). Phenomenology, on the other hand, investigates the lived experiences of people, making sense of their unique perceptions of their realities (Creswell, 2013; 2015). This paper seeks to understand social actions within hospital emergency rooms as they relate primarily to a patient with asthma as well as other patients with various other health conditions such as pregnancy, depression, arthritis, leg injury, etc. This study, comprised of a mini ethnography (Spradley, 1979, 1980) and phenomenological inquiry (Creswell, 2013; 2015), is limited in scope in that it focuses primarily on a single patient as she experiences emergency rooms at three different hospitals with acknowledgment of how five other patients said they felt about their lived experiences in one of the same emergency rooms as the asthmatic patient discussed in this paper.
This qualitative approach to research is consistent with other studies looking at the lived and cultural experiences of people from traditionally disenfranchised groups, according to Levitt et al. (2018), who also maintain that qualitative research is appropriate when focusing on issues that are “contradictory, problematic, or ill-fitting for a subpopulation.” Qualitative research enables scholars to address societal injustices and give voice to groups traditionally disenfranchised (Levitt et al., 2018).
The study started with ethnographic fieldwork, which entailed the asthma patient going to the hospital for legitimate medical concerns, such as breathing problems, and conducting participant observations. In addition to conversing with other patients, the asthmatic patient interacted with various hospital staff such as trauma nurses, doctors, lab assistants, physician assistants, medical interns, receptionists, triage nurses, charge nurses, patient advocates, hospital CEOs, security, paramedics, etc. During and after her visits, the asthma patient worked with patient advocates to assess the hospital cultures and make sense of encounters within those cultures. These advocates explained the procedures and helped her determine if she received adequate care. Participant observations enabled the patient to comprehend the cultural norms of each hospital and to study the social interactions while she also was being treated for asthma. Because she was required to wait so long to see a provider, she had ample time to interact with other patients and to notice additional communication taking place in the respective emergency waiting rooms.
Consequently, the present qualitative study entailed personal observations (Creswell, 2013; Fix et al., 2022) and in-depth interviews (Creswell, 2013) with a female asthmatic patient in conjunction with conversations/interviews with five other patients from the United States. This ethnographic and phenomenological work entailed multiple visits to hospitals and several interactions with healthcare professionals. While the adult asthmatic patient started being treated for asthma during her childhood well over 30 years ago, the bulk of the interactions discussed in the present paper focus on her interactions with healthcare professionals from 2020 to 2023. The patient, who is of Native American and African descent, discussed emergency room visits over 30 years, with the most salient experiences addressed in this paper encompassing interactions within the last three years. This woman went to the emergency rooms of different hospitals in the United States. She explains what transpired in three different emergency rooms: Hospital One, Hospital Two, and Hospital Three.
The asthma patient, serving as a participant observer, visited Hospital One three times over a three-year period, but only her most recent visit is addressed in this study. She had a single visit to Hospital Two and Hospital Three, and the salient themes from those visits are discussed below. Because the patient only went to the hospital when she actually was sick, she only had one visit to Hospital Two and Hospital Three, allowing her to authentically experience and discuss being a patient at each facility. However, subsequent communication with hospital staff about her visits took place by phone or email shortly after the respective visits. These conversations and interviews with hospital staff allowed her to ask questions about her visits while the issues were still fresh in her mind. Therefore, the patient ascertained greater insight about the respective cultures of the emergency rooms via interactions with hospital staff and other patients. Ultimately, involving stakeholders in ethnographic research offers a unique perspective on the social phenomenon (Watts-Englert et al., 2014). Watts-Englert et al. (2014) maintain that collaborating with stakeholders during ethnography in corporate research can enable human-centered innovation and lead to better ways of working together.
During data collection, personal observations were documented. This methodology is consistent with approaches taken with similar research. Fix et al., (2022) maintained that:
Observation can elucidate phenomena germane to healthcare research questions by adding unique insights. Careful selection and sampling are critical to rigor. Phenomena like taboo behaviors or rare events are difficult to capture. Observation provides unique information about human behavior related to healthcare processes, events, norms, and social context. Behavior is difficult to study; it is often unconscious or susceptible to self-report biases. Interviews or surveys are limited to what participants share. Observation is particularly useful for understanding patients’, providers’, or other key communities’ experiences because it provides an ‘emic,’ insider perspective and lends itself to topics like patient-centered care research.
Notes from personal observations and thick interview descriptions were analyzed until no new themes emerged. The goal was to identify the salient themes that captured how the individuals depicted in this study experienced healthcare professionals, illuminating the organizational communication that transpired so scholars and practitioners could make sense of those encounters. A qualitative research methodology was appropriate for this study, given that this approach was employed in similar studies (Creswell, 2013). After careful analysis, patient encounters were categorized and explained.
FINDINGS
The purpose of this study was to answer the following research questions: 1) How do patients experience healthcare professionals? 2) How do patients from traditionally disenfranchised groups experience hospitals and/or emergency room cultures? 3) What tactics can patients in this study employ to combat marginalization within healthcare systems? All of those research questions are addressed in this section.
Thematic analysis revealed that the asthmatic woman had a history of encountering marginalization from healthcare professionals. From childhood into adulthood, she was delayed in getting the medical assistance she needed. Her efforts to secure healthcare services were frequently met with resistance.
Background
A woman of Native American and African descent was born on the South Side of Chicago. She and her family resided in a few different homes in Chicago, but one particular home they occupied overlooked a lake. She lived in a high-rise apartment on the lakefront, and her family enjoyed a beautiful view of Lake Michigan. The view from her parents’ bedroom was the best one in the house. However, her memory of the warm and cozy condo was about more than just the great view. She recalled the many asthma attacks she and her siblings suffered while living there.
During her childhood, she and her siblings constantly had asthma attacks. When her parents dialed 911 to request an ambulance, to their dismay, the ambulance never came to their front door. The driver consistently parked several blocks away from their home because the Caucasian/White paramedics were terrified of entering the predominately African American/Black community on the South Side of Chicago. The 911 operator instructed the family to go outside to look for an ambulance. The ambulance driver was so afraid to be in the area that he turned his lights off, hiding from would-be predators, which made the ambulance more difficult for the sick child and her parents to find in the middle of the night.
On two separate occasions, when ambulances were called to the residence because the children were having asthma attacks, the paramedics failed to come to the front door. The family was expected to walk 10 to 15 minutes, looking for a parked ambulance with lights out. Most people take for granted the privilege of being able to call an ambulance and arrive at the designated destination promptly. This family was appalled that the paramedics feared their community, so the parents stopped dialing 911 when the children suffered asthma attacks. It was faster for the parents to take turns taking the children to the hospital in the family car. Over the years, that family made numerous trips to Michael Reese Hospital in Chicago.
Research suggests that the adverse experiences this family had with healthcare professionals are not unusual. Snyder et al. (2023) revealed that treatment from healthcare professionals tended to be better when healthcare professionals shared and understood the culture and values of the patients. In other words, African American/Black patients tended to live longer and enjoy higher quality care when treated by African American/Black doctors, according to Snyder et al., (2023). The Caucasian/White paramedics who were dispatched to treat the asthmatic little girl had such a negative view of the neighborhood in which the family resided that their perception of the community compromised their ability to provide adequate care. Perhaps African American/Black and/or Native American paramedics should have been sent. If the children had died of asthma, the family could have sued the ambulance company for failure to render services during an emergency. The paramedics were not in imminent danger. There was no threat precluding them from providing service to children of African and Native American descent. They sat outside for 15 minutes before announcing themselves. On one occasion, the child’s mother saw them down the street parked with their lights off, but she did not realize they were there for her child because they were so far away. The mother dialed 911 again to ascertain how long she needed to wait for an ambulance. That is when she learned that an ambulance had already been dispatched and that she needed to go outside with her asthmatic child and walk 10 to 15 minutes in the cold to locate the vehicle. The ambulance was not reasonably close, and the parents contemplated driving their child to the ambulance. Once, when the ambulance parked too far away, the parents canceled the ambulance and drove the child to the hospital themselves. During her childhood, this little girl made several trips to the hospital due to asthma, broken bones, and other minor issues.
Now, more than 30 years later, this child, who was born in Chicago, is a grown woman living with asthma. From time to time, she continues to suffer asthma attacks that require a trip to the emergency room. Her ongoing need for emergency care is consistent with the findings of Hargreaves, et al., (2019), who suggested that patients with adverse childhood experiences or traumas spent more time in emergency rooms during adulthood. The impact of trauma seemed to have long-term impacts on health. Moreover, these patients came to emergency rooms because they often lacked sustained relationships with primary care providers.
Nevertheless, from 2020 to 2023, this woman went to the emergency rooms of a few different hospitals in the United States. In each instance detailed below, the healthcare providers neglected her, ignored her, or discriminated against her in some fashion. Below is her account of what transpired in three different emergency rooms: Hospital One, Hospital Two, and Hospital Three.
Hospital One
Due to shortness of breath, the patient, who has historically suffered from asthma, used her inhaler, and she tried to go and see a doctor. The patient first attempted to visit a primary care doctor and an urgent care center before being told she needed to visit an emergency room where they were better equipped to treat her. The primary care doctor and the urgent care center manager maintained that they did not have the tools to care for her adequately. They informed her that they would have to send her to another facility for examinations and testing and that her results would not be ready for several days. Therefore, the primary care physician urged the patient to go directly to the emergency room, where she could enjoy a more timely and comprehensive examination and treatment. Taking the advice, the woman made her way to the nearest emergency room.
The asthmatic patient entered Hospital One early that evening, but it would be more than 15 hours before she actually got to see a doctor. Most of her time was spent in the waiting room, feeling ignored and neglected. Other patients were coming and going, but she sat there hour after hour, waiting for care. She could barely breathe, so she tried to talk as little as possible. She relied on text messages as well as paper and pencil to communicate because it allowed her to conserve her oxygen. She knew she was probably having an asthma attack, but she wanted to be seen by a doctor just in case something else was wrong. It was the time of year when asthmatic people tended to get sick. According to the Asthma and Allergy Foundation of America (AAFA), “Asthma attacks spike throughout September because it is high ragweed season, with ragweed pollen from 17 species of the wild, green plant filling the air… Ragweed can also trigger asthma attacks” (Asthma and Allergy Foundation of America, 2020). She suffered asthma attacks in September and October, which landed her in the emergency room.
This hospital visit started with the emergency room nurse taking her vitals. When she complained of chest pains and difficulty breathing, the nurse immediately ordered a COVID-19 test, a chest x-ray, an electrocardiogram (EKG), a test that helps to assess the health of one’s heart, and other tests. The nurse wanted to rule out a heart problem, which had never been an issue for the patient in the past. In addition to the EKG, the nurse took multiple blood samples and urine, all of which were sent to the lab for testing. Then, the patient was sent back to the lobby to wait to see a doctor. Hours went by, but still no doctor. The patient thought she had been forgotten, so she went to the nurse’s station to inquire about the status of her care. She was told that no doctor had signed up to see her. The nurse explained that patients were prioritized based on the severity of their illnesses and the time spent waiting in the hospital. However, this patient had been waiting hours, and she had difficulty breathing. The inability to breathe is typically regarded as a serious problem. Nevertheless, the patient, who contemplated leaving the hospital due to neglect, continued to wait.
The asthmatic patient observed other patients entering and leaving the emergency room before she did. She was discouraged by what seemed to be negative differential treatment, but she found solace in a group of other patients also sitting in the waiting room. One small group of African American/Black women sat together comparing notes. The African American/Black patients collectively determined that they were waiting longer than other patients entering the emergency room. Out of curiosity, they started inquiring about the nature of other people’s visits. When they got to the asthmatic woman, she told them she was there due to difficulty breathing. An African American/Black woman in her 30s said her stomach was hurting and that she had an obstructed bowel. She later learned while at the hospital that she was pregnant. Another African American/Black woman in her 50s had issues with arthritis and her joints. An African American/Black man had a leg injury. An elderly African American/Black woman did not sit near the asthma patient, but that senior citizen and the asthma patient encountered each other leaving the hospital, which is discussed later in this paper. (The elderly lady complained of a long wait and no treatment.) An openly gay, Caucasian/White man in his 30s was there suffering from depression stemming from an unwanted divorce. He said the breakup took him by surprise. He was visibly upset because his marriage, which lasted less than one year, had ended. The depressed man needed to talk, so he befriended the African American/Black women sitting next to him, including the asthmatic woman. He had been there at the hospital less time than anyone, but he got to see the doctor first. He was in and out in no time. When his visit was over, he came and sat by the women he had befriended before seeing the doctor, keeping them company while they waited. He said his visit was short and that the doctor prescribed him an antidepressant and encouraged him to see a counselor. Anyway, several people were waiting to see a doctor, but the Caucasian/White patients seemed to be treated first, even when they entered the hospital after patients of other races.
The nicely dressed asthmatic woman kept going to the nurse’s station every few hours to inquire about how much longer she needed to wait. She was told that her test results were ready, and that the hospital needed a doctor to see her. However, none of the doctors took her case, which the triage nurse and front desk clerk explained. The triage nurse had properly classified her care as a high-priority asthmatic case, but that designation did not expedite the patient’s care. The hours kept going by as she watched other patients come and go, most of whom were Caucasian/White. The other patients did not look as sick as she was, but who knows why they were in the emergency room. A layperson cannot adequately assess people’s health by merely looking at them as they sit in the emergency room
The nicely dressed asthmatic woman kept going to the nurse’s station every few hours to inquire about how much longer she needed to wait. She was told that her test results were ready, and that the hospital needed a doctor to see her. However, none of the doctors took her case, which the triage nurse and front desk clerk explained. The triage nurse had properly classified her care as a high-priority asthmatic case, but that designation did not expedite the patient’s care. The hours kept going by as she watched other patients come and go, most of whom were Caucasian/White. The other patients did not look as sick as she was, but who knows why they were in the emergency room. A layperson cannot adequately assess people’s health by merely looking at them as they sit in the emergency room.
The nurse at the nurse’s station tried to expedite the care for the asthmatic woman by going back there and reminding the doctors that an asthmatic woman was waiting. However, that did not help. The asthmatic patient continued to wait several more hours. More than 15 hours had passed, and she still had not seen a doctor. She sat in the emergency room overnight, waiting for a doctor to see her while her Caucasian/White counterparts were coming and immediately getting help.
After spending the night in the waiting room, the doctor finally called the patient after she had expressed concern about being neglected. The patient was then put on a gurney in the crisis unit, where she waited another hour and a half to two hours to see the doctor. At least now she could stretch out and nap a little while waiting. When the doctor finally entered the room, his attitude was negative, and his staff members were rude. The doctor who came in to see the asthma patient rushed her. He and his intern spent only a few minutes talking to her before returning to the office across the hall. They never discussed the results of her EKG. They did not give her the lab results even though the nurse told her the results were ready. After the doctor and his intern left the asthmatic patient, they could be heard gossiping about the patient, who was still across the hall on the gurney. The doctor said the patient looked fine to him and that he did not know why she was there. This physician also was heard commenting about whether the patient was some auditor who was there to check up on the hospital. The asthmatic patient was not an auditor. She was there because she was sick. The doctor released the patient without treating her. The comment was made by his staff that “He didn’t want to treat a nigger.”
It was clear that the doctor knew how the patient looked prior to calling her back for care. The doctor could see a picture of the patient next to her name on the portal used to track patients. The patient noticed that when she went up to the nurse to inquire about how much longer she needed to wait. When the nurse pulled up the patient’s name, her picture appeared. The picture of the patient was taken from her government- issued identification provided during registration. Therefore, the healthcare professionals knew exactly what their patients looked like before treating them, and they scanned hospital bracelets before conducting all tests to help ensure that test results were properly assigned to the right patients. This action enabled healthcare professionals to see in person and via computer-mediated communication who they were treating or would be treating. The disadvantage of having the photos beside the patients’ names was that it more readily allowed healthcare professionals to discriminate against patients based on appearance, such as race, gender, or something else.
After the doctor left the asthmatic patient, he and his intern could be heard gossiping. In addition to erroneously assuming the asthmatic patient was a hospital auditor, he made unsolicited remarks about the depressed, gay, Caucasian/White man who had already left the hospital at that point. The doctor said if his spouse had left him, he would not give his spouse the satisfaction of seeing him cry about it. He said he would be on Facebook kissing someone else. He also spoke of the fact that the man had only been married less than one year, yet he was crying like he’d lost a lifelong friend. The doctor seemed to be insinuating that the gay patient who was grieving the loss of his husband due to divorce was too sensitive. Gossiping about that patient might be deemed a violation of his rights. While the doctor did not discuss the patient’s diagnosis, which would definitely be a violation of the Health Insurance Portability and Accountability Act (HIPPA), commenting about a patient within earshot of another patient is unethical and incites distrust among patients who hear the gossip.
The asthma patient was still sick even though the doctor had cleared her to leave. The hospital demanded that she make room for another patient on the gurney, but her care was incomplete. Before discharging the asthma patient, a healthcare specialist wanted to make sure that she knew how to properly administer albuterol, her asthma medication, from the inhaler with a spacer to help ensure that more of the medicine entered her lungs. When a nearby nurse overheard the healthcare professional instructing the patient on how to utilize the spacer correctly, the offending nurse started making jokes about the patient. The nurse laughed at the patient and asserted that someone who has had asthma her entire life should already know how to use an inhaler and a spacer. The patient knew how to use an inhaler. The device that was relatively new to her was the spacer she now needed to enhance the effectiveness of the inhaler. Nevertheless, the offending nurse attempted to create a hostile environment for the asthma patient by blatantly laughing at her and making demeaning remarks. Laughing at a patient in the emergency room was rude.
As the asthma patient collected her things to leave, the nearby nurse said, “Sorry about the racism.” Another nurse who entered the room told the patient that she was a nurse and that she was not supposed to give EKG results to a patient but that she had noticed some abnormalities on the EKG. The patient’s heart was not getting enough oxygen, which explained the shortness of breath. The asthma attack had caused an abnormal EKG, which the doctor failed to address. The nurse also said she saw other issues from the EKG results. The patient was deficient in vitamins, such as potassium, needed for her heart to function properly. The doctor never mentioned this. Another nurse came in and listened to the asthmatic patient’s lungs, and he reported hearing wheezing. The doctor failed to address this as well. The nurse who heard the wheezing pointed out that he was not a doctor and did not have the authority to diagnose her, but he acknowledged that it was evident that the patient was sick. Consequently, the patient asked for a breathing treatment for asthmatics, something she had been accustomed to getting at Michael Reese Hospital during her childhood in Chicago. This treatment required the nurse to place a mask over the patient’s face and administer asthma medicine from a machine. The treatment was immensely helpful, but the patient had to ask for it. Had she not suggested it, the breathing treatment would not have been administered.
The doctor pretended the patient was fine, so he did not have to treat the asthmatic woman. Some of the nurses apologized for his rudeness and racism. It also was evident that the doctor did not appear devoted to caring for the asthmatic patient. Moreover, as the patient was on the gurney, she could hear the doctor chitchatting with his intern about matters unrelated to patient care. They did not appear to be in a rush to see other patients, so the doctor could have taken the time to discuss test results and care with the asthma patient. The healthcare professionals had sufficient time to treat the patient, but it was not a priority for some of them. Many of the staff members back there were standing around not doing much. Some were seen surfing the Internet. Appalled by what she was witnessing and experiencing, the patient asked the healthcare provider, “Why did it take so long to see a doctor? I have been sitting in the waiting room since yesterday, waiting for you.”
Not everybody was rude. The male nurse administering the asthma treatment was kind to the patient. The patient spoke to him about the rude nurse laughing at her and talking about her. The male nurse explained to the patient that the nurse harassing her had a certain rare skill that the hospital needed, which was why they had tolerated her unprofessional conduct for so long. He said she had a history of being rude to patients who were not Caucasian/White. The male nurse said the disrespectful nurse was known for trying to start disputes with African American/Black patients so that she could get them trespassed from the hospital. Fortunately, the asthmatic patient never spoke directly to the rude nurse. She merely commented about the offending party to the male nurse helping the patient.
Then, when the asthmatic lady was about to leave the hospital, she requested a letter documenting her illness to explain why she had been away from her normal duties for over 24 hours. These notes are customary in the healthcare profession, but the doctor told the nurse to tell the patient he was refusing to provide one. This prolonged the patient’s stay because she appealed the doctor’s refusal to provide a note. The asthmatic woman waited patiently while the doctor and his team gave the patient her discharge papers and a doctor’s note. Only after the asthmatic patient said she wanted to speak with a manager or chief of staff did a nurse finally enter the room and offer to provide a note. The patient wanted the doctor’s note to indicate when she arrived at the hospital and when she left, but the hospital refused to document that. The note only documented the day the patient left the facility. It failed to show that the patient had been in the hospital since the previous day, waiting for treatment.
As the asthmatic patient was exiting the premises of the hospital, she encountered a dark-skinned, elderly African American/Black woman who was on her way back home. The woman said she had left the hospital without help. She said they refused to treat her and that they also refused to provide her with medical records from previous visits. This woman said she was in pain. She said hospital staff threatened to trespass her if she kept asking for help. She said they would not answer her questions or address any of her medical issues. The woman, who appeared to be in her 70s, relied on public transportation, and she had elected to go to that particular hospital because it was the closest one to her house. That patient sought emotional support from the asthmatic patient as they were leaving the hospital. After a long wait, the elderly woman said she was denied care by the hospital, and she conveyed those concerns to the patient with asthma. The asthma patient asked the woman if she thought a patient advocate from the hospital would be of greater assistance to her. The elderly woman said she intended to call the hospital when she got home, so she could speak to one.
While the asthmatic patient may have been neglected by hospital staff, the other patients from the waiting room were quite attentive. The other patients offered emotional support. They exchanged phone numbers in the hospital and started texting each other about their care or topics to discuss with hospital staff. For example, that patients would go and get nurses for each other. In another instance, one patient encouraged the asthmatic woman to request food or snacks given her long wait because other patients had been given snacks. When a patient got something from hospital staff, such as water or a snack, that person would return to the waiting room and encourage other patients to request the same. The patients also made space for each other in the waiting room to stretch their legs on multiple chairs. The asthmatic patient and a man with a leg injury obtained extra legroom, which allowed them to be more comfortable while they waited. The patients interacted with hospital staff on behalf of the asthmatic patient by asking for minor favors, such as a blanket to stay warm while they waited. Sometimes, they asked how long they needed to wait to see a doctor. Finally, after leaving the emergency room, the patients checked to see if each other made it home safely from the hospital. Some contacted each other after the visit to offer additional emotional support.
Hospital Two
While at Hospital Two, the asthmatic patient spent very little time waiting in the emergency room before initial contact with healthcare professionals. She went to the hospital due to difficulty breathing, which stemmed from allergies and asthma. She was taken back and given initial care within minutes of arriving at the hospital. Then, the triage nurse sent her back to the waiting room before the hospital had her return to staff for subsequent care. After the initial contact, the patient waited an extended period of time in the emergency room for follow-up care. While in the waiting room another African American/Black woman, who was coughing profusely and not wearing her mask, sat near the asthmatic patient. The woman informed the asthmatic patient of her struggles with the hospital. She said she’d been there several times trying to get care, but nobody knew what was wrong with her. She had returned to the hospital numerous times for treatment to no avail. Due to the woman’s coughing, the asthmatic patient relocated to a more comfortable seat with less pollution, and she continued to wait for her name to be called by the doctor.
This hospital also did lab work on the patient, which was bizarre. One nurse stuck a needle in the patient’s arm for what felt like an eternity. This nurse kept sticking the patient with a needle like she was practicing on her, so the patient asked for a different healthcare professional. After the arduous task of collecting her blood, the nurse dropped the vial of blood. According to hospital policy, once blood work has been improperly handled, it has to be discarded. However, the nurse picked it up and was going to attempt to use it. From the looks of it, had the patient not requested a new specimen, the bad one may have been used. Fortunately, the hospital collected a second sample at the patient’s request.
The patient returned to the waiting room to await the test results. This time, the wait was longer. Then, a nurse called the patient’s name. As the patient collected her things to follow the nurse who had called her, the nurse got angry and walked away hastily, leaving the patient. The patient could barely slide beyond the heavy security doors, which required a key to access. Once back there, the asthmatic patient did not know where to go because the nurse had left her. The nurse was mad because the patient moved too slowly for the fast-walking nurse.
Uncertain of where to go, the patient approached the nurse’s booth and asked for assistance. They located the nurse who had called the patient. When the nurse arrived, she approached the patient and abruptly cut off the patient’s hospital identification bracelet. The patient was baffled because the doctor had not yet seen her, nor had she been given her test results. The nurse accused the patient of being a reporter. The patient maintained that she was not a reporter. That hospital was in litigation with someone, and the nurse thought the patient was there to covertly investigate. The patient had no idea about the legal battle and was at the hospital because she was sick. She was not there as a reporter.
The patient was legitimately sick, so a healthcare professional prescribed some allergy medicine for her. However, the prescription was written for the wrong pharmacy. When the patient noticed this, she asked for help from the same nurse’s station she had gone to for directions earlier. However, a Caucasian/White, male nurse behind the desk replied, “I do not have to answer your questions anymore because you have been released.” The male nurse refused to help the patient, and he did not want to call the previous nurse back over either. Only after the patient asked to speak with a manager or the chief of staff did the nurses suddenly decide to assist the patient by correcting her prescription. Overhearing that the patient wanted to file a grievance, a patient advocate rapidly approached the patient to ensure she had what she needed.
Part of the problem with this hospital visit was that the nurse was in such a rush that she prematurely released the asthmatic patient. The patient was released prior to the completion of her care. She had been told before going back to the waiting room after an examination and testing that she would see a doctor, but the nurse released the patient before the patient saw the doctor. The patient advocate offered to readmit the patient, but they were able to conclude their business without that.
As the patient was getting ready to leave the hospital, she scanned her release papers, looking at her test results. Some of the tests the healthcare professional had ordered should have been reported. It turned out that the technicians had “forgotten” to order some of the tests the physician’s assistant had instructed them to perform. Had they neglected her intentionally, or was this an honest oversight?
The Asian physician’s assistant who treated the patient told the patient he thought some nurses were jealous of her. He told the patient she was pretty and that he overheard the technicians who had been instructed to complete her lab work debating on what her race must be. They were commenting about her pretty hair, trying to determine her race from her hair texture. Given all the blood they took from her, they could have determined her race from blood test results, but they forgot to test her blood. The technicians forgot to perform some of the tests the healthcare professionals ordered. As a result, the patient was waiting for lab results from tests that had never been conducted. They took her blood, but they did not run the tests. Consequently, she left the hospital without test results. This failure to complete tests compromised the quality of care the hospital provided. Overall, Hospital Two rushed and neglected the asthmatic patient, but the hospital’s patient advocate mitigated the damages by immediately offering support when the patient asked for it.
Hospital Three
Hospital Three did not have an unusually long waiting time for initial emergency room care. Within an hour of arriving, the patient was taken back and given a chest x-ray and an EKG, blood work, and other tests. The patient knew she was experiencing allergies and asthma, but the doctors still examined her thoroughly to rule out other illnesses. While the patient knew what was wrong with her, the doctor still had to follow protocol for care just in case the patient was wrong.
The treatment at this hospital started off fine. However, in their haste to treat the patient, they lost the first two vials of blood drawn from her. Then, they asked the patient to give subsequent samples after she had already been waiting a long time for the analysis from the first test. This time, they took seven or eight vials of blood for simple tests, which usually require one or two vials. The request for additional blood raised a red flag for the patient. Her first question was whether something was wrong. However, they quickly explained to her that the lab indicated that her blood samples never made it to them. Therefore, she needed to give new samples. It seemed as if these healthcare professionals just wanted her blood.
The Asian doctor who treated the patient told her he was going to have a cardiologist check her out, but he later canceled that request. He had intended to run some tests, but after the good EKG results, he declined to run any subsequent tests on the patient’s heart. He determined that her heart was not the problem. Asthma is a lung disease, and it does not currently appear to be having an adverse influence on her heart. At this point the patient merely needed to wait for test results, so she could be cleared to return home, but those results did not arrive in a timely manner.
The patient’s primary complaint about this hospital was that they were slow to post lab results, and she was unsure why they needed so much of her blood. The patient experienced some uncertainty because the healthcare providers did not adequately explain their actions. Her first question was why they needed so much blood given the simple tests they were performing. There was talk of a third party wanting her blood, but nobody ever obtained her consent to give her blood to a third party. When she later asked the hospital president about the matter, he commented that his team always complied with the demands of law enforcement. However, nobody presented a search warrant or told the patient that anyone wanted her blood. It was a violation of HIPPA for the hospital to give the patient’s blood to a third party if that is actually what transpired. Now, the patient was concerned that her blood had not been lost earlier but that she was being manipulated by a third party who wanted it.
When the patient inquired about the test results, she was told that no news was good news. When something is wrong, the hospital contacts patients immediately. If they did not contact you, then nothing about your results alarmed them. However, the actual results offered more peace of mind to the patient. The EKG results were good, and all other labs were good. However, the hospital needed to provide information faster. The tests are only meaningful if patients know the results.
The hospital’s tardiness in providing test results compelled the patient to speak with a patient advocate and the hospital’s CEO as suggested by hospital staff. These administrators collaborated to ensure that the patient’s results were provided to her long after she had already been released from the hospital. The president told the patient that the delay was due to an external audit that caused them to be understaffed. He said his team was normally more attentive, but the audit required so much time that it took his team longer to complete simple tasks. Overall, Hospital Three was slow to follow up with the patient, but the CEO and a patient advocate helped expedite the process days after the patient had gone home.
THEMATIC ANALYSIS
After analyzing the asthmatic patient’s visit to three different emergency rooms, the patient’s experiences can be classified into the following categories: 1) Long wait times, 2) Poor and Unprofessional Attitude / Disrespectful Communication, 3) Neglect, 4) Feeling Rushed, 5) Having to Ask for Care, 6) Discrimination, and 7) Support from Patient Advocates.
Long wait times
At Hospital One, the asthmatic patient had to wait overnight for treatment that should have been rendered immediately upon entering the hospital. The asthmatic patient said, “What is taking so long? I’ve been waiting overnight to see a doctor?” The inability to breathe is a severe medical emergency that warranted the prompt attention of healthcare professionals. Other patients with less severe healthcare challenges were treated prior to her. The other hospitals were slow to offer medical test results.
This finding was consistent with research by Ehrler et al., (2016). The time spent in an emergency waiting room before care can shape how patients perceive care. Patients are satisfied when healthcare professionals offer updates about wait times. If hospitals can tell people approximately how long they may have to wait before being treated, this may reduce uncertainty, according to Ehrler et al., (2016).
Long wait times can be a barrier to treatment as some people do not have the patience to wait long. Hoyer et al., (2019) stated that the door-to-doctor duration was the primary reason neurological patients with headaches, seizures, or other issues left emergency rooms prematurely. Some patients left before the start of care, and others left before care was completed due to long wait times in emergency rooms. One hour was deemed to be the golden wait time for patients. Waiting longer than an hour or two for care was considered excessive (Spechbach et al., 2019), based on a study of 500 patients.
Finally, the openly gay, Caucasian/White man had a shorter wait time than the patients who were African American/Black. However, given the level of anxiety and depression the Caucasian/White man seemed to be experiencing, it’s possible that the hospital wanted to intervene as early as possible to prevent a possible suicide or to treat him before he left the hospital without seeing someone for his illness. This is consistent with the research of Alakeson et al., (2010) who asserted that mentally ill patients often left hospitals without treatment because of long wait times in emergency rooms. While the patient depicted in the present study did not mention suicide in the waiting room, suicide, unfortunately, is sometimes what results from severe depression that goes untreated. Long wait times can be a barrier to care, and the extended stays in emergency rooms can diminish the perceived quality of care from hospitals.
Poor and Unprofessional Attitude / Disrespectful Communication
The asthmatic patient encountered poor and unprofessional attitudes as healthcare professionals indicated that they did not want to “treat a nigger.” A nurse apologized to the patient for the racism she suffered. Moreover, the patient was teased by a Caucasian/White, female nurse for needing to be told how to properly use a spacer, which is a device that is attached to her inhaler, to ensure that more of her medicine enters her lungs. These attitudes were congruent with the findings of Ming et al., (2019). Ming et al. (2019) indicated that “uncompassionate attitudes, unprofessional communication, disrespect of patient rights, and unsatisfactory quality of nursing care” were the salient themes emerging from complaints by patients. When patients are not treated with dignity, they tend to have a problem. Patients expect respectful communication.
Another example of poor and unprofessional attitudes and/or disrespectful communication emerged from the unsolicited communication about an openly gay Caucasian/White man. This male patient said, “I was so happy,” as he cried about the shock of his relationship ending. He didn’t see the divorce coming. He came to the hospital because the breakup was causing him to have difficulty concentrating at work because he was so distraught. However, hospital staff could be heard gossiping about him. They made comments about his extreme level of distress given that he had been married less than one year. The doctor also stated what he would have done if his spouse had left him. The attitude of the doctor toward the patient could have been more professional. Fortunately, the patient was not present to witness the negative remarks. However, other patients overheard healthcare professionals talking about him.
Neglect
When patients are in excruciating pain or suffering from breathing problems, they tend to feel neglected when they have to wait overnight for care. In this way, long wait time can cause patients to perceive that they are being neglected. A man with a leg injury was in a lot of pain at Hospital One, and he frequently complained about the long wait as he rolled around the waiting room chairs in agony. Similarly, the asthma patient at Hospital One was left overnight in the waiting room unattended with a diminished capacity to breathe, which felt like neglect. The only benefit to the extended stay in the emergency room was that she made friends with other patients who came and sat by her in the emergency room. The other patients kept her company and made requests to healthcare professionals on her behalf. For example, one patient beside her helped her with small tasks, such as asking for water or a blanket. Therefore, while the patient may have felt neglected by hospital staff, she was comforted by other patients who offered support.
The failure of hospitals to conduct tests that were ordered by doctors can easily be construed as neglect. Healthcare professionals neglected to perform tests that were ordered, or they misplaced the patient’s vials of blood, requiring healthcare professionals to request subsequent blood tests after the patient had already waited hours for the first tests to be processed. This kind of interaction compromised the care offered to the asthmatic patient. It also extended her wait time as the hospital would have to call her back to conduct additional testing, which they forgot to perform the first time. The good news is that they did retest the patient or take a second sample when they lost something. Re-testing merely prolonged the patient’s wait time and added to perceptions of neglect.
Finally, the patient was neglected by the doctor at Hospital One, who had medical information about her that he failed to share, such as the results of her EKG and chest x-ray. She learned of her results from a person at the hospital who was unauthorized to share the information. She also ascertained more insight into her health from the discharge papers containing EKG and other test results. This enabled her to study the numbers to help determine her level of health.
The other patients complained of neglect. An elderly African American/Black woman, who was leaving the hospital around the same time the asthma patient did, was profoundly disappointed in the hospital for failing to treat her. She said: “Girl, they wouldn’t even see me. They didn’t do anything for me. And they said they would trespass me if I didn’t leave and quit trying to get admitted.” The older woman complained of how poorly she was treated there. She said they refused to treat her and failed to provide medical records from past visits, which she formally requested multiple times. This type of neglect has been reported by Ryan et al., (2011), who maintained that elderly patients tend to experience more adverse treatment and negative outcomes than younger patients. Emergency rooms need to be safe spaces for elderly patients.
Finally, patients must not be ignored in emergency rooms. Patients die there all the time, and healthcare professionals need to be prepared to care for them before they expire, according to Kongsuwan et al., (2016). This neglect could be due, in part, to poor triage or assessments of health when patients first enter emergency rooms (Spechbach et al., 2019). Because patients are prioritized based on the urgency of their needs, the level of care required, and the length of time they have been waiting in the hospital, poor assessments can cause patients to be given too high or too low a priority. When patients in critical care are deemed to be a low priority, these patients are delayed in getting the care they need. When marginalization is factored into the equation, wait times can be longer.
Feeling Rushed
After waiting in the emergency room overnight, the patient had to ask for an asthma treatment after she was finally called back to see the doctor at Hospital One. The doctor was in such a rush that he neglected to address the primary reasons for the visit. He should have informed her of the chest x-ray and EKG results, which staff said only a doctor was authorized to convey. He had medical information about her that she needed, but he neglected to offer it. After the doctor left, the patient felt hurried by the staff who tried to rush her out of the hospital before treating her. While the patient breathes normally today, at the time of her visit, she was alarmed by the inability to function as usual. “I don’t have enough oxygen to talk normally,” she explained. She notified the doctor of her inability to breathe well, but he tried to release her even though her test results showed a lower-than-normal oxygen level. Because of the diminished breathing capacity, the patient asked for and was given a breathing treatment by the nurse long after the doctor left the room and tried to discharge the patient without treatment. Healthcare professionals also tried to rush the patient out of the door without a doctor’s note, but the patient insisted on having one before she left the premises.
Similarly, the nurse at Hospital Two was in such a hurry that she angrily left the patient. Then, she provided the patient with discharge papers prior to the completion of her care. These papers had the wrong pharmacy information, and it was evident from the papers that certain test results needed to be included. The patient said feeling rushed was an understatement, and the same concern was articulated by other patients (John et al., 2021). Feeling rushed was a theme that emerged in the research of John et al., (2021), who studied pregnant women. Ultimately, patients had more negative perceptions about their quality of care when they felt rushed by healthcare professionals or when healthcare professionals seemed indifferent about caring for them.
Having to Ask for Care
The asthmatic patient was having difficulty breathing, and EKG results from Hospital One indicated that the patient’s heart was not getting enough oxygen. The doctor should have done something about this, but he ignored the patient’s concerns. He did not take her complaints about the inability to breathe seriously, or perhaps he did not care. “May I have a breathing treatment,” the patient asked. The patient asserted herself and requested a breathing treatment, which the nurse administered. Patients at all three hospitals had to assert themselves to get the treatment or service they wanted. For example, the patients went up to the nurse’s station to find out what was taking so long. They asked for food, water, blankets, expedited care, etc. Some services, such as asthma treatment, may not have been rendered had they not been requested.
DISCRIMINATION
Discrimination was a theme that emerged. The doctor from Hospital One reportedly did not want to “treat a nigger,” so he ignored the patient’s inability to breathe. Moreover, a Caucasian/White female nurse tried to antagonize the patient with harassing comments designed to provoke her to do something that would get her trespassed. The Caucasian/White, male nurse who administered the patient’s breathing treatment informed the patient that this particular Caucasian/White, female nurse was known for starting disputes with African American/Black patients, so she could get them trespassed from the hospital. Harassment and microaggressive behavior have been noted in the work of others (Johnson & Johnson, 2019; South et al., 2020). South et al. (2020) asserted that African American/Black providers and patients were subjected to microaggressions in healthcare, and most of those encounters went unreported. Harassment and derogatory name calling were implied as some of the insults and dismissals Harvard University psychiatrist Chester Pierce, who coined the term microaggressions, said were regularly inflicted upon African Americans/Blacks by people who are non-African American or non-Black (Johnson & Johnson, 2019). South et al., (2020) recommended accountability systems for reporting racism so meaningful feedback and intervention could help inspire better conduct. They also urged healthcare professionals to reevaluate policies to ensure that they are not inherently racist. Reorganize organizational power structure to eradicate racism. Appoint leaders to oversee anti-racist efforts. Launch training to teach anti-racist conduct. Empower people to address racism.
The asthmatic patient, whose test results revealed that her oxygen levels were too low, was made to wait an unusually long time as her Caucasian/White counterparts were treated prior to her for illnesses that appeared to be less severe. For example, a Caucasian/White man suffering from depression came to the emergency room after the asthmatic woman and was treated long before she was. While depression can be a major illness, the man presenting with depression, stemming from a recent breakup with his husband, did not appear to be having problems breathing. However, he was immediately treated and released. To the hospital’s credit, patients suffering from mental distress need to have reduced wait times so that they do not leave the hospital prior to being treated (Alakeson et al., 2010). This decreases the likelihood that they would leave the hospital and kill themselves or end up in jail for something (Alakeson et al., 2010). It is possible that the hospital prioritized his care because they did not want to take a chance on him killing himself or going into greater distress as he sat in the noisy waiting room.
This finding was consistent with the assertions of Kyerematen et al., (2023), who indicated that anti-Black racism was prevalent in the field of medicine. Anti-racism communication strategies need to be employed to promote equality for African American/Black patients. Some healthcare professionals have created a communication tactic to promote greater equality in response to the racism against African American/Black patients. “Presence 5 (P5)” is a communication framework designed to promote meaningful connections with patients through five practices: Prepare with Intention, Listen Intently and Completely, Agree on What Matters Most, Connect with the Patient’s Story, and Explore Emotional Cues.” (Duncan et al., 2022). Clearly, “Clinician adoption of anti-racism communication language may promote racial justice in clinical interactions and positively influence patient care and health outcomes through meaningful yet challenging dialogue on the impact of racism on patients’ health” (Duncan et al, 2022). Because racism compromises the health of African American/Black people in general, not just patients (Bird et al., 2021), conscientious healthcare professionals may want to consider adopting communication strategies that promote greater equality.
Support From Hospital Patient Advocates and Other Patients
The final theme that emerged was that the asthma patient got better care when she relied on patient advocates or when she asked to speak with an advocate. The patient got used to saying: “May I speak to a manager or the chief of staff.” She essentially was requesting an advocate. At one of the hospitals, the patient worked directly with a patient advocate assigned by the hospital to get what she needed. For example, when the hospital discharged the patient prematurely at Hospital Two, a patient advocate helped the patient send her allergy prescription to the correct pharmacy. The advocate also invited the patient to be readmitted so she could speak directly to a doctor, but she was able to get what she needed without being re-admitted. At Hospital Three, the patient advocate and hospital CEO ensured that the patient’s test results were released to her. The results were ready but had yet to be distributed to the patient. The CEO said the hospital’s tardiness in getting the results to the patient was due to an audit requiring the hospital’s immediate attention.
In addition to the bonafide patient advocates provided by the respective hospitals, the asthmatic patient in the current study got support from other patients in the emergency room. At Hospital One, the other patients offered her emotional support. They encouraged her to ask for food and water because she had been waiting so long to see a doctor. The patient made space for her to stretch her legs out and relax on multiple chairs. They interacted with hospital staff on her behalf by asking for a blanket for her to stay warm, and they called healthcare professionals over so she could ask how much longer it would be before she would have an opportunity to see a doctor, etc. The patients checked to see if each other made it home safely from the hospital. They contacted each other after the visit to offer additional emotional support.
Overall, the salient themes that emerged in this study were: 1) Long wait times, 2) Poor and Unprofessional Attitude / Disrespectful Communication, 3) Neglect, 4) Feeling Rushed, 5) Having to Ask for Care, 6) Discrimination, and 7) Support from Hospital Patient Advocates and Other Patients. These findings from the present study parallel those of Funk (2022), who revealed the following about African American/Black patients: 1) They had to speak up get help, 2) Pain was not taken seriously, 3) Felt rushed by healthcare professional, 4) Felt like they were treated with less respect than other patients, 5) Felt that their quality of care was less than what other patients received, 6) Judged due to weight, and 7) Health concerns were not taken seriously. Arguably, the health concerns of the asthmatic patient in the present study were not taken seriously by the doctor at Hospital One because he left without treating her. She had to ask a nurse to give her an asthma treatment. Essentially, many of the themes in the study by Funk (2022) were prevalent among interactions for the asthmatic patient and other patients in this study.
Clearly the cultures of the emergency rooms in this study rendered patients from traditionally disenfranchised groups marginalized. For example, treatment of the African American/Black women in this study was delayed or denied. In other instances, the women had to ask for service that should have been a customary part of the care, such as with the asthmatic woman needing to ask for a breathing treatment. Moreover, the derogatory comments and blatantly disrespectful conduct exhibited by hospital employees toward African American/Black women subsequently compromised their perceived quality of care. As for the openly gay, Caucasian/White man, he was promptly treated when he entered the emergency room. However, healthcare professionals could be heard gossiping about him and making fun of him for being distraught by the loss of his husband. The doctor may have been in violation of HIPPA by openly discussing this patient, or at the very least the doctor’s actions were in poor taste. Ultimately, the hospital cultures depicted in this study may not offer patients from historically marginalized groups the best possible experience. The values espoused by the hospital employees and leaders reflected in this study suggested that little regard was placed on the quality of care of the patients represented in the current study. Hospitals either did not take the concerns of patients seriously or they did not care. Even when medical professionals had scientific evidence of illness, such as low oxygen levels as revealed by EKG results, doctors still attempted to deny care or diminish the quality of treatment. Future research needs to ascertain if similar findings are present within other populations or with other individuals from traditionally disenfranchised groups. Subsequent research should also explore how healthcare professionals are socialized (Gates, 2009; 2023a).
One place to start the conversation about socializing healthcare professionals might be with the work of Gates (2009; 2023a; 2023b). She discussed the socializing experiences of nearly 150 professionals and the role communication played in the ongoing process of learning the ropes. Coleman (2023) also emphasized the importance of clear communication to overcome racial inequities in healthcare, which remains a concern. Extrapolating from the organizational socialization model by Gates (2009; 2023a; 2023b), as shown below, socialization may play a pivotal role in how healthcare professionals interact with patients and other healthcare professionals. If healthcare professionals are taught to treat certain segments of the population differently, these differences could render some patients as well as certain members of the healthcare profession marginalized. Perhaps future research could explore how healthcare professionals are socialized into healthcare organizations and how healthcare professionals are socialized to interact with patients. Additional research also could examine how patients are socialized into healthcare organizations, identifying strategies to enhance their experiences. It’s imperative to explore how patients are socialized into healthcare organizations because many patients need more effective tactics to overcome marginalization in healthcare. People entering healthcare professions for treatment need training on what to do and where to go when their rights are violated. Future research could focus on other segments of the population within healthcare to spur more effective socialization of healthcare professionals to help eradicate the marginalization of patients.
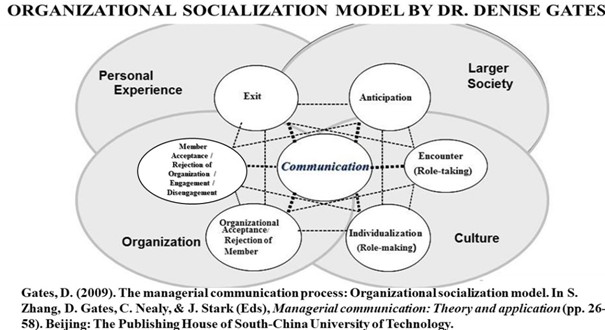
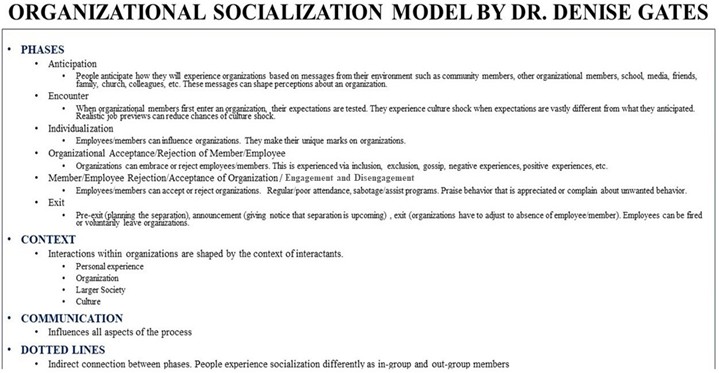
CONCLUSION
From ethnographic and phenomenological perspectives, this exploratory study examined the encounters of a woman from a non-dominant racial group as she interacted with healthcare professionals at three different hospitals in conjunction with making sense of the lived experiences articulated by five other patients who were treated at Hospital One during the same time the asthma patient was there. The hospital cultures reflected in this study rendered patients from traditionally disenfranchised groups marginalized. Treatment for patients from non-dominant racial groups was delayed or denied, and in the case of an openly gay, Caucasian/White male, healthcare professionals made fun of his situation, which conveyed a lack of professionalism.
Experiences reflected in this study were consistent with the lived experiences of other disenfranchised groups (Karaduman et al., 2023; Ming et al., 2019). Patient concerns with healthcare professionals can be classified into the following categories: 1) Long wait times, 2) Poor and Unprofessional Attitude, 3) Neglect, 4) Feeling Rushed, 5) Having to Ask for Care, 6) Discrimination, and 7) Support from Hospital Patient Advocates and Other Patients. While the asthmatic patient in this study contended with a few challenges at each hospital, she often overcame them with assistance from other patients and/or patient advocates provided by the respective hospitals. The various advocates helped ensure that healthcare professionals adhered to hospital standards and upheld the rights of patients.
This study is limited. It cannot be generalized to other populations because it relied primarily on the self- report data from one patient living with asthma and her accounts/interviews with five other patients in the same emergency room as the asthmatic patient. While memories are not 100 percent accurate, people tend to recall critical incidents that played a pivotal role in their care. More importantly, the detailed accounts of the patients’ lived experiences with healthcare professionals in three different hospitals offer enough context for readers to ascertain if transferability is possible. Finally, thematic analysis in the present study is consistent with other research results, and these findings substantiate a need for subsequent reflection on how people from traditionally disenfranchised groups experience healthcare systems. Moreover, a more in-depth analysis of how healthcare professionals are socialized into organizations (Gates, 2023a) that treat patients may be an opportunity to identify areas for healthcare professionals to augment their skills when it comes to interacting with patients. While limited, this study adds value to the extant research on communication with healthcare professionals.
REFERENCES
- Acar, B.A. (2018). Impact of emergency room meetings on the improvement of door-to-needle times in acute ischemic stroke patients: A single center’s experience. North Clin Istanb, v. 5, n. 4, p. 282–287. DOI: 14744/nci.2017.00378. PMID: 30859157; PMCID: PMC6371987.
- Alimohammadi, H., Hatamabadi, H., Khodayari, A., Azimi, M. (2019). Medicine specialists in forensic medicine files; a cross sectional study. Archives of Academic Emergency Medicine, v.7, n. 1, e11, pp. 1-5.
- Asthma and Allergy Foundation of America (2020). The danger of September’s asthma peak is here. https //community.aafa.org/blog/for-people-with-asthma-the-danger-of-peak-week-is-here.
- Banerjee, A., & Sanyal, D. (2012). Dynamics of doctor-patient relationship: A cross-sectional study on concordance, trust, and patient enablement. Journal of Family Community Medicine, v. 19, n. 1, pp. 12-19. Doi: 10.4103/2230-8229.94006.
- Berthelot, S., Lang, E., Messier, A. (2020). Sending low-acuity patients away from the emergency department – An imperative for appropriateness and integration. CJEM, v. 22, n.5, p. 638–640. DOI 10.1017/cem.2020.430.
- Bird, C., Webb, E., Schramm, A., Torres, L., Larson, C., deRoon-Cassini, T. (2021). Racial discrimination is associated with acute post-traumatic stress symptoms and predicts future post-traumatic stress disorder symptom severity in trauma-exposed Black adults in the United States. Journal of Traumatic Stress, v. 34, p. 995–1004.
- Center for Disease Control and Prevention (2023). Racism and health. In https://www.cdc.gov/%20minorityhealth/racism-disparities/index.html.
- Center for Disease Control and Prevention (2023). Asthma. https://www.cdc.g ov/nchs/fastats/asthma.htm#print.
- Center for Disease Control and Prevention (2023). Most recent national asthma data. https //www.cd c.gov/asthma/most_recent_national_asthma_data.html.
- Coleman, C. (2023). Health care policy and law: Health literacy and systemic racism—using clear communication to reduce health care inequities. JAMA Internal Medicine, v. 183, n. 8, p. 753-754.
- Creswell, J. W. (2013). Qualitative inquiry and research design: Choosing among five approaches. Thousand Oaks, CA: Sage.
- Creswell, J. W. (2015). A concise introduction to mixed methods research. Thousand Oaks, CA: Sage.
- Creswell, J.W., Klassen, A. C., Plano Clark, V. L., & Smith, K .C.(2011). Best practices for mixed methods research in the health sciences. Washington, DC: National Institutes of Health. http: /dx.doi.org/10.1037/ e566732013-001.
- Creswell, J.W., & Plano Clark, V. L. (2011). Designing and conducting mixed methods research (2nded.). Thousand Oaks, CA: Sage.
- Duncan, N., Cox, J., Shankar, M., De Leon, G., Baratta, J., Brown-Johnson, C. & Zulman, D. (2022). “I Will Listen”:Ttransdisciplinary anti-racism communication dialogue adapted to medicine. The Annals of Family Medicine, p. 3264; DOI: https://doi.org/10.1370/afm.20.s1.3264
- Dyer, C. (2023). Doctors raise concerns about possible discriminatory action against trainee who was suspended after patient complaint. BMJ, v. 381, p. 1252. http://dx.doi.org/10.1136/bmj.p1252.
- Ehrler, F., Siebert, J., Wipfli, R., Duret, C., Gervaix, A., & Lovis, C. (2016). Improving patient experience in pediatric emergency waiting room. Nursing Informatics. p. 53 -539, Doi:10.3233/978-1-61499-658-3-535.
- Elsevier, (2020). Female millennial patient perspectives in the emergency department: A qualitative analysis. American Journal of Emergency Medicine, v. 38, 2462–2464.
- Fix GM, Kim B, Ruben M, McCullough MB. (2022). Direct observation methods: A practical guide for health researchers. PEC I nov, 100036. doi: 10.1016/j.pecinn.2022.100036. PMID: 36406296; PMCID: PMC9670254.
- Funk, C. (2022). Black Americans’ views about health disparities and experience with health care. Pew R search Center. https // pewresearch.org/science/2022/04/07/black-americans-views-of-and-engagement-with-science/ps_2022-04-07_black-americans-science_03-09/.
- Gates, D. (2023a). Leveraging organizational socialization to enhance employability. International Journal of Research and Social Science, v.7, n. 11, pp.1519-1551.
- Gates, (2023b). Managing stress and overcoming traumatic workplace betrayals. In Perspectives on stress and wellness management in times of crisis. Edited by Bansal, Rohit, 51–62, Hershey, PA: IGI Global.
- Gates, D. (2010). Polarity management: Balancing stress and tranquility polarities during a Business Research Yearbook, v. XV11, n. 2, p. 704-711.
- Gates, D. (2009). The managerial communication process: Organizational socialization model. In S. Zhang, D. Gates, C. Nealy, & J. Stark (Eds), Managerial communication: Theory and application, (pp. 26-58). Beijing: The Publishing House of South-China University of Technology.
- Ghandakly, E, & Fabi, R. (2021). Sterilization in U.S. immigration and customs enforcement’s (ICE’s) detention: ethical failures and systemic injustice. AJPH,111, n. 5, p. 832-834.
- Glerada, C. (2019). Clare Gerada: We need a complaints code of conduct. BMJ, p. 364, n. l59 doi:10.1136/bmj.l59.
- Guimond, E., Getachew, B., Nolan, T., Sheffield-Abdullah, K., Conklin, J., Hirschey, R. (2022). Black patients with cancer and their oncology clinicians: exploring factors that influence outcome disparities. Oncology Nursing Forum, v. 49, n. 6, p. 509–524. DOI 1 .1188/22.ONF.509-524.
- Gupta, R., Agrawal, R., Bukhari, K. Jabbar, A., Wang, D., Diks, J., Alshal, M., Emechebe, D., Brunicardi, F.C., Lazar, J., Chamberlain, R., Burza, A. & Haseeb, M.A. (2021). Higher comorbidities and early death in hospitalized African-American patients with Covid-19. BMC Infectious Diseases, v. 21, n—78 at ps://doi.org/10.1186/s12879-021-05782-9.
- Hargreaves, M., Mouton, C., Liu, J., Zhou, Y., Blot, W. (2019). Adverse childhood experiences and health care utilization in a low-income population. Journal of Health Care for the Poor and Underserved, v.30, n.2, pp. 749–767. DOI:h tps://doi.org/10.1353/hpu.2019.0054.
- Haywood, C., Diener-West, M., Strouse, J., Carroll, P., Bediako, S., Lanzkron, S., Haythornthwaite, J. Onojobi, G., Beach, M. (2014). Perceived discrimination in health care is associated with a greater burden of pain in sickle cell disease. Journal of Pain and Symptom Management, v. 48, n.5, p. 934-943.
- Hoyer, C., Stein, P., Alonso, A., Platten, M. and Szabo, K. (2019). Uncompleted emergency department care and discharge against medical advice in patients with neurological complaints: a chart review. BMC Emergency Medicine, v. 19, n. 52. D I: ttps://doi.org/10.1186/s12873-019-0273-y.
- John, JR, Curry, G., Cunningham-Burley, S. (2021). Exploring ethnic minority women’s experiences of maternity care during the SARS-CoV-2 pandemic: a qualitative study. BMJ Open 2021;0:e050666. doi:10.1136/ bmjopen-2021-050666.
- Johnson, N. & Johnson, T. (2019). Microaggressions: An introduction. In Thomas, U. (Ed.), Navigating microaggressions toward women in higher education (pp. 1-22). IGI Global. https:doi.10.4018/978-1-5225-5942-9/ch001.
- Jones, R.A., Hirschey, R., Campbell, G., Cooley, M.E., Lally, R., Somayaji, D., Gullatte, M.M. (2021). Update to 2019–2022 ONS Research agenda: Rapid review to promote equity in oncology healthcare access and workforce development. Oncology Nursing Forum, v. 48, n. 6, p. 604–612. https //doi.org/10.1188/21 .ONF.604-612.
- Karaduman, M., Hocaglu, A., Sabak, M., Zengin,S., (2023). Analysis of the complaints of the patients and their relatives to healthcare professionals. Journal of Contemporary Medicine, v.13, n. 1, p. 72-77. DOI:10.16899/jcm.1218472.
- Kyerematen, B., Garcia, R., Cox, J., Zulman, D., & Shankar, M. (2023). Moving beyond inquiry: a secondary qualitative analysis on promoting racial justice in clinical care. BMC Medical Education, 23, n. 180, https://doi.org/10.1186/s12909-023-04131-5.
- Levitt, H., Creswell, J., Josselson, R., Bamberg, M., Frost, D., Suarez-Orozco, C. (2018). Journal article reporting standards for qualitative primary, qualitative meta-analytic, and mixed methods research in psychology: The APA publications and communications board task force report. American Psychological Association, v..73, n.1, p.26–46. http: /dx.doi.org/10.1037/amp0000151.
- Lindlof, T. & Taylor, B. (2011). Qualitative communication research methods. United Kingdom: Sage Publications.
- Ming, Y., Wei, H., Cheng, H., Ming, J., Beck, M. (2019). Analyzing patients’ complaints awakening of the ethic of belonging. Advances in Nursing Science, 42, No. 4, pp. 278–288.
- National Center For Health Statistics (2023). National hospital ambulatory medical care survey: 2021 emergency department summary tables. https //www.cdc.g ov/nchs/data/nhamcs/web_tables/2021-names-ed-web-tables-508.pdf
- Ryan, D., Liu, B., Awad, M. & Wong, K. (2011). Improving older patients’ experience in the emergency room: the senior-friendly emergency room. Aging Health, v. 7, n. 6, p. 901–909.
- Shea, S, Misru, D., Ehrlich, M. Field, L, Francis, C. (1992). Correlates of nonadherence to hypertension treatment in an inner-city minority population. American Journal of Public Health, v. 82, n.12, p. 1607-1612.
- Snyder, J., Upton, R., Hassett, T., Lee, H., Nouri, Z., Dill, M. (2023). Black representation in the primary care physician workforce and its association with population life expectancy and mortality rates in the U.S. JAMA Network Open, v. 6, n. 4, e236687. DOI:10.1001/jamanetworkopen.2023.6687
- South, E., Butler, P., & Merchant, R. (2020). Toward an equitable society: Building a culture of anti-racism in health care. The Journal of Clinical Investigation, v. 130, n. 10, p 5039–5041.
- Spradley, J.P. (1979). The ethnographic interview. New York, NY: Holt, Rinehart, &Winston.
- Spradley, J.P. (1980). Participant observation. New York, NY: Holt, Rinehart, & Winston.
- Spechbach1, H., Rochat, J., Gaspoz, J., Lovis, C., and Ehrler, F. (2019). Patients’ time perception in the waiting room of an ambulatory emergency unit: a cross-sectional study. BMC E ergency Medicine, v 19, n. 41. h tps //doi.org/10.1186/s12873-019-0254-1.
- Vrettos, B. (2023). Communicate, collaborate, and document: the pillars to avoid and manage complaints. South African Orthopedic Journal, v. 22, n.1, p. 6–7.
- Watts-Englert, J., Szymanski, M., Wall, P., & Sprague, M. (2014). Collaboration for impact: Involving stakeholders in ethnographic research. International Journal of Business Anthropology, v. 5, n. 1, p. 55–69.
- White-Goyzueta, K, Gates-Mayweathers, D., & Nance-West, O. (2023). Exploring religiosity and the reflective perspectives of microaggressions endured by students and educators from non-dominant racial groups in higher education. International Journal of Research and Innovation in Social Science, v. 7, n. 11, p. 770-792.
ABOUT THE AUTHOR
Dr. Denise Gates-Mayweathers is a business professor, prolific author, and talent optimization consultant, specializing in organizational socialization and strategic management. Dr. Gates has an earned doctoral degree as well as a post-doctorate in organizational communication and management. A graduate of the University of Missouri-Columbia, Dr. Gates is known for her organizational socialization model, which was published in a textbook by the Publishing House of South China University of Technology and utilized by MBA students. A 2023 publication about her organizational socialization model offered the salient themes that emerged from the examination of the lived experiences of nearly 150 professionals from various industries. That empirical research supported Dr. Gates’ existing framework on organizational socialization, and it illuminated a variety of workplace betrayals designed to impede career success. Dr. Gates has authored and co-authored a plethora of academic publications over the years, and her research has been presented at national and international conferences. Ultimately, Dr. Gates is inspired to help organizations draw the greatest value out of people with her research, instruction, and consulting.

