Sign up for our newsletter, to get updates regarding the Call for Paper, Papers & Research.
Support Supervision for Community Health Workers in Uganda: Implications of Village Health Teams in Mitooma District
- Augustino Ngabirano
- Mathew Chibunna Igwe
- 2259-2275
- Feb 19, 2024
- Health Education
Support Supervision for Community Health Workers in Uganda: Implications of Village Health Teams in Mitooma District
Augustino Ngabirano1* & Mathew Chibunna Igwe2
1,2Department of Public Health, School of Allied Health Sciences, Kampala International University, Ggaba Road Kampala
*Corresponding Author
DOI: https://dx.doi.org/10.47772/IJRISS.2024.801165
Received: 18 January 2024; Accepted: 20 January 2024; Published: 19 February 2024
ABSTRACT
Background: Support supervision for Community Health Workers is a field that is undervalued worldwide. The performance of Uganda’s Community Health Workers, also known as Village Health Teams, is impacted by their lack of supportive supervision. This study evaluated the impact of support supervision on VHT involvement in community-based healthcare in Uganda’s Mitooma area.
Method: This article’s empirical analysis is based on data gathered between September and October 2021 from 341 Village Health Teams from eight Sub-counties in the Mitooma area as part of a cross-sectional study. Data were gathered via semi-structured questionnaires, focus groups, and key informant interviews. STATA version 14.2 was used for descriptive analysis, and manual methods were used for qualitative (thematic and content) analysis.
Results: In Mitooma district, support supervision is still dispersed even though it is thought to be a tool for encouraging Village Health Teams, facilitating continuing training, and keeping them accountable for their work. Lack of funds, irregular supervision, and a lack of guidelines were among the challenges limiting support supervision in the district.
Conclusion: It was generally acknowledged that support supervision is still undervalued in the VHT program. Stakeholders suggested that in order to solve these issues, there should be more financing, supervisor job descriptions that are explicit, and in-person supervisory meetings.
Keywords: Village Health Teams, Support supervision, Mitooma district, Kampala International University
INTRODUCTION
Support supervision of Community Health Workers (CHWs) is a crucial component and road to enhancing CHWs’ ability to function in healthcare efficiently in order to achieve Universal Health Coverage (UHC), a significant aim of many nations. However, it is an understudied field globally (1). Due to a worldwide scarcity of medical specialists, particularly in low- and middle-income nations (LMICs) (2) strengthening primary health care (PHC) systems through increasing CHW capacity is gaining traction (3). Community health workers (CHWs) are dependable community members with less medical training who may offer basic healthcare services, health promotion, and health education (1; 4). The World Health Organization and United Nations support CHW initiatives as a crucial tactic to improve health outcomes, especially in resource-constrained settings. These programs have shown successful in a variety of nations and health domains (5; 6). However, in some contexts, implementation challenges still make CHW programs less effective (2; 7; 8). With varying degrees of success, Uganda, a low-income nation according to the World Bank, has tried to undertake CHW projects. There are just 0.2 physicians for every 1,000 people in the nation, indicating a severe scarcity of qualified healthcare workers (2; 9). Since 75% of people live in rural regions, it is especially harder to guarantee that those in most need have access to healthcare (3).
In Uganda, community health workers, also known as Village Health Teams (VHTs), are volunteer health care providers who were implemented in 2001 as a model for providing primary healthcare to local communities (10). In Uganda, CHW supervision is dispersed and faces a number of difficulties, including inadequate funding and issues with the structure and design of the supervisory framework (4). To tackle these issues related to public health, the Ugandan Ministry of Health (MOH) established Village Health Teams (VHTs) in 2001. These teams are made up of community members who volunteer their time without formal pay (1; 10; 11). Numerous duties were assigned to VHTs, such as illness surveillance, home visits, common health condition management, and health promotion (10). However, due in large part to inadequate training, inadequate oversight, and a reliance on volunteerism, the program proved to be unsustainable and unproductive (1; 11; 12). The term “community health worker” is therefore used to mean laypeople engaged in health promotion, prevention, and/or delivery (13). While CHWs play a variety of context-specific functions, they are primarily employed in their local communities and are part of the formal health system, which is run by NGOs or the government, but they lack tertiary education or a paraprofessional degree (14).
The World Health Organization (WHO) released a report in 2018 that evaluated areas that were seen to be essential to enhancing and improving CHW programs (15). These aspects included supervision, pre-service training, compensation, community involvement, and selection. The study came to the conclusion that, despite the literature’s emphasis on supervision, this particular field has received little attention, and it rated the strength of the available evidence for supervision as “weak.” (16). One significant obstacle is that, when used in reference to healthcare personnel, the phrase “supervision” has varied definitions and conceptions (17). It frequently includes “supportive, managerial, and clinical supervision,” among other aspects’ (18) each of which employs a unique strategy and objective. “A process that involves monitoring work processes, understanding the causes of problems and providing possible solutions, as well as general management,” is how supervision has traditionally been understood in the health care industry’ (19). While it has also been claimed that supervision could have a more caring and supporting role, this definition places greater emphasis on the responsibility and monitoring components of supervision in order to improve health services.
In fact, more and more recently, helpful monitoring has been prioritized (20). For instance, particular to CHW, (21) imply that enhanced CHW cohesion, confidence, community recognition, and a sense of belonging to the healthcare system should all be facilitated by supervision. Numerous studies have identified difficulties in the implementation of supervision, in addition to differences in its definitions and conceptualization. Not only is there insufficient data regarding what constitutes appropriate CHW supervision (17; 20), but there is also variability in supervisory interactions across different geographical contexts various initiatives, which has prevented the creation of best practices or uniformity (22). Therefore, research on the role of CHW supervision, how it is implemented, and strategies for facilitating efficient delivery is required (6; 23).
AIM AND OBJECTIVES
The purpose of this research was to evaluate the support supervision provided to VHTs at the district level in western Uganda’s Mitooma area and investigate the connection between support supervision and VHT involvement in community-based healthcare. Specifically, we aimed to understand;
- How support supervision is viewed and understood by VHTs in Mitooma district
- How VHT supervision currently is provided in Mitooma district
- The difficulties that currently surround VHT supervision in Mitooma district
MATERIALS AND METHODS
Study design
This study combined semi-structured interviews with a quantitative survey as part of an exploratory mixed methods research design. The data analysis is based on chapters four and five of my master’s dissertation, “Assessment of Village Health Teams’ Participation in Community-Based Healthcare and Associated Factors in Western Uganda: A case study of Mitooma district,” which was completed in September and October 2021 at Kampala International University in the public health department under the guidance of Dr. Andrew Tamale. In order to examine the relationship between support supervision and VHT performance in community-based healthcare, this study relied on a cross-sectional survey that included VHTs (n = 341), facility-based health staff (n = 5), and key stakeholders involved in VHT supervision, such as VHT coordinators (n = 9). Additionally, a study of the literature was done using three electronic databases that are often used in the domains of public health and related fields (PubMed, Web of Science, and Global Health) as well as Google Scholar for grey literature.
Study Setting
The survey was carried out between September and October of 2021 in Mitooma district. There are about 183,444 people living in the Mitooma district in western Uganda’s Ankole sub-region; 93.8 percent of them are subsistence farmers (24). A parliamentary act established the district, which commenced operations on July 1st, 2010. The district is made up of multiple administrative divisions, including Counties/Constituencies (n = 3), Sub-counties and Town Councils (n = 18), parishes and wards (n = 77), and villages/cells (n = 565). Prior to that, the district was known as Ruhinda County and was a part of the larger Bushenyi district. Mitooma district shares boundaries with Rukungiri district to the west, Bushenyi district to the north, Sheema district to the east, and Ntungamo district to the south. There are two health centers II, eight health centers III, and one health center IV in the district, which is presently being converted into a district hospital. Acute lower respiratory infections, malaria, HIV/AIDS, urinary tract infections, and diarrhea are the top five infections reported in the district (25; 26).
Due to the researcher’s familiarity with the major players in the community health care delivery system in the area—having lived and worked there for a number of years—the study was conducted in the Mitooma district for accessibility considerations. Uganda’s decentralization regulations mean that district-level policy-making, prioritization, and execution of health care are mostly carried out. Under this arrangement, the District Health Team (DHT) of the Mitooma District Health Office (DHO) supervises the operation of VHTs attached to Health Center IIIs. Numerous partners, including national and international non-governmental organizations (NGOs), support the DHO by offering assistance with daily operations and VHT training. The nonprofit organization known as Action for Community Development (ACODEV) is presently providing support to the greatest number of VHTs in the district. With the goal of reducing unwanted pregnancies, maternal and infant deaths, unsafe abortions, teenage fertility, and total fertility to enhance the wellbeing of individuals, families, and communities, the NGO collaborates directly with the Mitooma DHO to support and train VHTs in health education and health promotion regarding contemporary family planning techniques (27).
Study population and sampling technique
The study was carried out on 341 adult VHTs chosen from the VHT population (n=594) in the eight purposively selected Sub-counties of Mitooma district, including Kiyanga, Bitereko, Rurehe, Katenga, Mayanga, Nyakizinga Kashenshero Town council, and Mitooma Town council. A multi-stage and probability proportional to size (PPS) sampling technique was used in this investigation. The study unit consisted of a VHT; however, the focus group discussions (FGD) participants also comprised VHTs, the DHT coordinator, health workers (VHT focal persons), and members of the community. The study participants included VHTs who had been active in their rural communities for a year prior to the research and were identified by community mobilizers and local leaders in the study sub-counties. There are 1198 VHTs in the Mitooma district, which are dispersed throughout 18 Sub-counties, 62 parishes, and 557 villages (24). The study employed a multi-level non-exhaustive sampling technique to ensure that the attributes to be measured had the least degree of variability, the highest levels of precision and confidence, and internal and external validity (Table 1).
Table 1. List of Sub-counties with number of parishes, villages and VHTs: probability proportional to size (PPS)
| Region | Sub-county | No. of Parishes | No. of
Villages |
No. of
VHTs |
Relative
frequency (rf) |
Study sample
(PPS) |
| 1 | Kiyanga S/C | 5 | 48 | 96 | 0.17 | 55 |
| Bitereko S/C | 5 | 47 | 94 | 0.16 | 54 | |
| 2 | Kashenshero T.C | 4 | 15 | 30 | 0.05 | 17 |
| Rurehe S/C | 4 | 39 | 78 | 0.13 | 45 | |
| 3 | Katenga S/C | 4 | 58 | 116 | 0.19 | 67 |
| Mitooma T/C | 4 | 15 | 30 | 0.05 | 17 | |
| 4 | Mayanga S/C | 4 | 36 | 72 | 0.12 | 41 |
| Nyakizinga S/C | 4 | 39 | 78 | 0.13 | 45 | |
| Total | 34 | 297 | 594 | 1 | 341 | |
Source: Adopted from Mitooma District Health Records (2019)
Mitooma District was purposefully split up into four areas. Then, using a table of random numbers, two Sub-counties were randomly selected from each region to produce eight (8) Sub-counties. As shown in table 1 above, the number of VHTs to be included in the study from each sub-county was determined using probability proportional to size (PPS). A practical number of VHTs were specifically selected from each parish. Eight focus group discussions (FGDs), one in each of the eight Sub-counties that were targeted, and six key informant interviews (KIIs) with health center staff and VHT focal individuals were carried out during the study’s qualitative phase.
Data Collection and Procedure
Tools and techniques
A suitable number of VHTs were selected from each parish. The data gathered from a cross-sectional survey involving 341 Village Health Teams from eight Sub-counties in the Mitooma district during September and October 2021 is the basis for the empirical analysis of this study. To achieve the goal of comprehending the supervision delivery system as it currently exists in the Mitooma district we modified a survey created by Madede et al. (28) whose original form had been applied to assess a supportive supervision intervention for health professionals in Mozambique earlier.
Table 2. Tools and techniques used during data collection
| Research Question | Objective | Technique |
| (i) What are the socio-demographic features of VHTs in Mitooma district? | To examine the socio-demographic characteristics of VHTs and their influence on participation in community-based health care. | Data from Master’s thesis titled “Assessment of Village Health Teams’ participation in community-based health care and associated factors in western Uganda: a case study of Mitooma district.” |
| (ii) What are the VHT perceptions towards various stakeholders in Mitooma district? | To examine the VHT perceptions towards the health facilities, communities, government and NGOs in influencing their linking role in the district | Data from Master’s thesis titled “Assessment of Village Health Teams’ participation in community-based health care and associated factors in western Uganda: a case study of Mitooma district.” |
| (iii) How is support supervision perceived and conceptualized by VHTs and supervisors in Mitooma district? | To examine the understanding of VHTs regarding support supervision and to contextualize the variables surrounding it, including the need, duration and perceived supervisor. | Documentary search and in-depth interviews with key informants. |
| (iv) How VHT supervision is currently delivered in Mitooma district? | To examine the significance of support supervision including frequency, style and mode of delivery, and to investigate the ways in which these variables have impacted the participation of VHTs in health care programmes in the district | Documentary search and in-depth interviews with key informants. |
| (v) What challenges currently surround VHT supervision in Mitooma district? | To examine the factors limiting support supervision in the district and the possibilities to overcome them | Documentary search and in-depth interviews with key informants. |
Structured surveys
The data used in this paper comes from just three portions of the questionnaire that the VHTs completed: The first section asked questions about the sociodemographic characteristics of VHTs, such as age, gender, level of education attained, marital status, length of time spent living in the community, and the total number of years spent serving as a VHT. Questions addressing the practical aspects of VHTs’ perceptions of the many stakeholders impacting their engagement in the delivery of healthcare were asked in section two; questions regarding support supervision (type, duration, and frequency) were asked in section three.
Individual interviews
Semi-structured individual interviews were conducted with all major stakeholders to gather data on their perspectives of supervision and its obstacles. We decided to conduct individual interviews because we reasoned that VHTs would be more inclined to be candid in a one-on-one setting than in a group context where their supervisors would be present. The researcher created and tested semi-structured interview guides before using them. The principal investigator (PI) conducted interviews in English with district officials and NGO program managers, while one of two locally hired and trained research assistants (RAs) conducted interviews in Runyakitara, the language spoken by VHTs and facility-based health workers. At the time of the study, the people conducting the interviews were independent researchers; they were not working for the NGO funding the VHTs. The interviews were painstakingly recorded on paper, and an English transcription was done right away. The PI and the RA then reviewed the transcripts to make sure the translation process had preserved all of the meaning and to guarantee that they were clear and accurate. Participants were contacted as needed to address any unclear areas.
Data management
After the interviews and participant questionnaire replies, the RA organized, cleaned, and labeled the survey data before transferring it into Microsoft Excel for Windows 10. Subsequently, the data were exported into STATA version 14.2, where they underwent a thorough comparison and were ready for descriptive analysis. Frequencies, means, medians, and standard deviations were used in the descriptive analysis. Thematic and content qualitative analysis was performed by hand. Using an open-coding framework, initial codes were created by consulting the study questions again. Once the final collection of codes was generated, they were organized into themes and carefully examined to make sure they made sense and included evidence to support them.
Ethical considerations
Permission to perform the study was given by Kampala International University-WC’s IREC. Before any data was actually collected, permission to interact with VHTs was obtained from the Mitooma district’s Chief Administrative Officer (CAO) and District Health Authorities (DHO). VHT Supervisors and Local Council I Chairpersons deliberately selected eligible participants using methods that did not violate the beliefs, practices, or culture of the local community. After being thoroughly educated about the goal of the study and the risks and advantages of participating in both Runyakitara and English, study participants signed a written informed consent form to confirm that their participation was entirely voluntary.
RESULTS
Socio-demographic characteristics of study participants
This study involved 341 VHTs from 8 selected Sub-counties of Mitooma district. The majority of the VHTs 264 (77.4%) were female, with a mean stay duration of 27 years. Their mean age was forty-three years, and the majority of them had completed primary level 267 (78.3%). The majority of VHTs, 323 (94.7%), were married, and the average household size was seven members. According to the data, the majority of VHTs worked in crop agriculture, accounting for 264 (77.4%), and the majority of them had 332 (98.5%) cell phones (Table 2).
Table 2. Socio-demographic characteristics of VHTs (n=341)
| Variable | Attribute | Summary measure | |
| n(%) | Mean (sd) | ||
| Length of stay in community
in years |
1-10
11-20 21-30 31-40 41 and above |
16(4.7%)
96(28.2%) 119(34.9%) 64 (18.8%) 46(13.5%) |
27.3(12.1) |
| Sex | Male
Female |
77(22.6%)
264(77.4%) |
|
| Age in years | 18-28
29-39 40-50 51 and above |
22(6.5%)
121 (35.5%) 139 (40.8%) 59(17.3%) |
43.3(8.5) |
| Educational level | None
Primary Senior four Senior six Tertiary |
1(0.3%)
267(78.3%) 61(17.9%) 1(0.3%) 11(3.2%) |
|
| Marital status | Single
Married Divorced/separated Widowed |
2(0.6%)
323(94.7%) 1(0.3%) 15(4.4%) |
|
| Household size | 1-5
6-10 11 and above |
78(22.9%)
256(75.1%) 6(1.8%) |
6.7(1.8) |
| Occupation | Crop agriculture
Animal rearing Formal salaried earner Business Casual laborer |
264(77.4%)
12(3.5%) 2(0.6%) 61(17.9%) 2(0.6%) |
|
| Social status | LC leader
Religious leader Lay leader Other |
70(20.5%)
8(2.4%) 115(33.7%) 148(43.4%) |
|
| Own Cell phone | Yes
No |
332(98.5%)
59(1.5%) |
|
| Occupation before VHT position | Community based distributor
Traditional birth attendant Farmer Business Government employee NGO employee Student |
86 (25.2%)
5 (1.5%) 212 (62.2%) 37 (10.9%) 1(0.3%) |
|
Source: Primary data (2021)
VHT perceptions on different stakeholders
To gain an understanding of support supervision and how VHTs view it in connection to different stakeholders, an analysis was carried out (Table and Figure 3).
Table 3: Examining VHT perceptions on different Stakeholders (n=341)
| Perception on the Health system | SA | A | N | D | SD | Median |
| A high level of communication and feedback does exist among the health facility staff that VHTs report to | 92
(26.9%) |
101
(29.6%) |
35
(10.3%) |
45
(13.2%) |
68
(19.9%) |
2.000 |
| Adequate supervision and monitoring by the District authorities is made for the VHT programme | 43
(12.6%) |
34
(9.9%) |
33
(9.7%) |
172
(50.4%) |
59
(17.3%) |
4.000 |
| Perception on the Community members
Community members show positive involvement in VHT activities |
99
(29.0%) |
102
(29.9%) |
26
(7.6%) |
65
(19.1%) |
49
(14.4%) |
1.000 |
| Communities receive adequate supplies of medicines and health information | 57
(16.7%) |
45
(13.2%) |
13
(3.8%) |
124
(36.4%) |
102
(29.9%) |
4.000 |
| Values and perceptions in the community do not limit the implementation of VHTs activities among the community members | 155
(45.5%) |
95
(27.8%) |
15
(4.4%) |
41
(12.0%) |
35
(10.3%) |
2.000 |
| Perception on the Government and NGOs/Partners
Government and implementing partners/NGOs make satisfactory supply of basic materials and equipment to facilitate VHT members in doing their work |
69
(20.2%) |
45
(13.2%) |
9
(2.6%) |
102
(29.9%) |
116
(34.0) |
4.000 |
| Government and implementing partners have provided a satisfactory number of trainings and refresher courses for VHTs | 31 (9.1%) | 67
(19.6%) |
15 (4.4%) | 134
(39.3%) |
94
(27.5) |
4.000 |
| As VHT members we feel adequately supported financially to perform our tasks | 61 (17.9%) | 72
(21.1%) |
21 (6.2%) | 98
(28.7%) |
89
(26.1%) |
5.000 |
| Government policies relating to the VHT programme and the general health sector are favourable for the work of a VHT member | 132 (38.7%) | 154 (45.2%) | 8
(2.3%) |
26
(7.6%) |
21
(6.2%) |
4.000 |
| There exists an enabling political environment in the country for the VHT programme to proceed effectively | 123 (36.1%) | 152
(44.6%) |
9
(2.6%) |
30
(8.7%) |
27
(7.9%) |
2.000 |
Figure 1: Examinng VHTs Perception on different Stakeholders
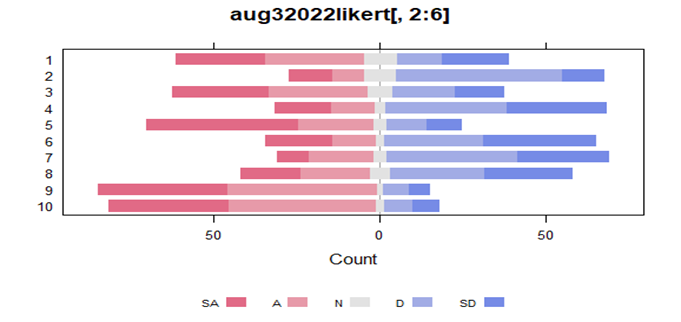
Regarding the health system, the majority of VHTs (30%) concurred that there was a great degree of feedback and communication among the employees of the health facilities they work with. On the question of district authorities providing them with sufficient support and supervision, the majority of 50% disagreed. The majority of community members—29.6%—agreed that there is beneficial community member involvement in their activities. Furthermore, 45% of respondents strongly agreed that the implementation of their actions could not be constrained by the values and perceptions of community members. 36% of respondents, however, did not feel that the communities were receiving enough supplies, medications, and health information from them. According to the majority of NGOs and the government, 45% of them felt that government initiatives benefited their work. The majority of respondents, or 45%, concurred that the program is operating in an atmosphere that is supportive of it. That being said, the majority of 29% strongly disagreed that there were enough supplies and tools to make their jobs easier. Even so, 39% of respondents disapproved of the quantity of trainings and refresher courses that had been provided.
Support supervision of VHTs in Mitooma district
The majority, 336 (98.5%), reported receiving supervision within the previous six months, while 5 (1.5%) reported not receiving any supervision at all. Out of 341 VHTs, 196 claimed to have had supervision from non-governmental organizations, while 145 said they had supervision from government employees. Of all VHTs, 231 (67.7%) reported that supervision sessions lasted longer than 60 minutes, while 110 (32.3%) reported that they lasted less time. A majority of 293 (86.4%) reported receiving supervision in person, whilst 46 (13.6%) reported receiving supervision over the phone. The majority, 183 (54%) said they had supervision for three months or less, and 156 (46%) said they had supervision for more than three months (Table 5).
Table 5. Support supervision of VHTs in Mitooma district
| Attribute | n(%) | 95%CI |
| Have you been supervised during the last six months? | ||
| Yes | 336(98.5) | 96.5-99.4 |
| No | 5(1.5) | 0.6-3.5 |
| Which entity supervised you? | ||
| NGO staff | 196(57.5) | 52.1-62.6 |
| Government / Health facility staff | 145(42.5) | 37.4-47.9 |
| Average duration (minutes) of supervision discussion | ||
| > 60 | 231(67.7) | 62.6-72.5 |
| ≤ 60 | 110(32.3) | 27.5-37.4 |
| What mode of supervision was used? | ||
| Face-to-face | 293(86.4) | 82.3-89.7 |
| Phone call | 46(13.6) | 10.3-17.7 |
| How often do you receive support supervision? | ||
| > 3 months | 156(46.0) | 40.8-51.4 |
| ≤ 3 months | 183(54.0) | 48.7-59.2 |
Source: Primary data 2021
Qualitative findings
The purpose of supervision
Three themes emerged from the stakeholder interviews about the perceived goals of supervision: (i) providing motivation; (ii) fostering accountability; and (iii) facilitating continuing education and training.
The motivational goals of supervision
Every stakeholder group mentioned that one goal of monitoring was to increase motivation. After getting supervision, VHTs felt respected and appreciated, which in turn extrinsically motivated them to keep doing community service. I feel encouraged and motivated by this monitoring, therefore I know that my efforts are valued. (Male VHT). Moreover, it gives us the impression that our managers cherish us and enjoy our work. (Female VHT) In a similar vein, supervisors from DHOs and NGOs saw supervision as a means of legitimately acknowledging VHTs, a recognition that they believed would encourage them to fulfill their community-based healthcare tasks.
Motivation exists. The VHTs will remark, “Oh District Officials came here, you are moving with this person!” if we find out. The “doctor of the village” is how they [VHTs] see themselves. They envision themselves collaborating with a few important individuals who value their contribution to the community. (District Official). Furthermore, it raises their spirits. “Look, these are those people [NGO staff], they know us,” [VHTs] think to themselves.(NGO Official)
The accountability purposes of supervision
The VHTs strongly believed that supervision served as a means of keeping people responsible for their job-related responsibilities, in opposition to its incentive goals. While the accountability goals of supervision seemed to drive VHTs to perform their work in order to avoid punishment, the motivational goals of supervision seemed to encourage VHTs to do their tasks in order to get positive reinforcement and a sense of appreciation. Because we are aware that we are constantly being watched, supervision encourages us to act without hesitation. (Female VHT)
The continuing education and training purposes of supervision
It was indicated that supervision plays a significant role in promoting continuous training across all stakeholder groups, including the development of new skills through the provision of constructive feedback to reinforce and improve practice. Stakeholders saw this goal of monitoring as a way to give professional development and ongoing education priority. Once more, under supervision, I learn new skills that I may share with the group. Typically, we communicate new information we learn via supervision with others. (Female VHT)
The fact that CHWs receive numerous trainings while under supervision also helps them to learn. As a result, they have the power to bring about constructive change in their specific settlements. (Worker in a Health Facility) working to this individual means recognizing their positive traits and positively fixing anything that is not working well. (District Official)
According to DHO authorities, supervisors may also help career growth because they will become more aware of each VHT’s unique leadership qualities through the process of offering supervisory support. I know you have the attributes of a leader, therefore if I were to supervise you, I could suggest you for professional advancement. (District Official)
Challenges impeding VHT supervision
The perceived difficulties impacting VHT supervision in this particular setting are the subject of this section. These difficulties include: (i) Insufficient resources to support supervision; (ii) Problems with the structure and design of supervision; and (iii) Disagreements amongst important parties participating in CHW supervision.
Insufficient funding to enable supervision
The main obstacle to providing VHT monitoring at the DHO level was identified as a lack of resources. According to DHO authorities, there was a decrease in the budget for VHT supervisory activities since the Ministry of Health had not provided enough funding for community health programs. Moreover, DHO representatives admitted that their own budgets did not adequately account for supervisory efforts. Even when you include investment, the Ministry of Health’s funding for these initiatives is minimal. They believe that community service is unimportant. It certainly needs to be prioritized, and without adequate funding, the ensuing oversight wouldn’t occur or run smoothly! (District Official).
Problems with the supervision’s layout and organization
Regarding the difficulties with the structure and design of supervision, all parties involved made comments. DHO authorities proposed that practical issues such a shortage of medical professionals to take on supervisory duties and a lack of clear standards and training for supervision were the main causes of implementation difficulty. The specifics of what a supervisor should investigate are not specified by the system. And that has to do with following the rules. I promise you that there are lacking criteria for supervision. (District Official). However, in the event that you are without a medical professional, who can provide the supervision? Because how can you have more people to do supervision if there aren’t even enough [workers] in the facility? (District Official). Employees at the health facility cited the high supervisee-to-supervisor ratio as a roadblock to providing supervision. Because there aren’t as many of us supervisors as there are regions that need to be supervised, our work is pretty incompetent. We still have a ton of VHTs in other regions to work on, so it takes us a while to go back and supervise the ones we previously observed. (Health Facility Worker)
The extensive distances required getting supervision, the inadequate communication between supervisors and CHWs, the infrequency of supervision, and the absence of individual supervision were among the issues that CHWs also identified with relation to supervision. Alright, the center is quite a distance away. We must ride a boda-boda, a local motorcycle, there and we are not compensated. It is financially costly. (Female VHT). In a group setting, we are unable to ask them specific questions. (VHT in Male) Some recommendations for enhancing oversight Aside from that, stakeholders offered recommendations on ways to enhance oversight. i) More financing; and ii) Modifications to the structure and design of the supervisory system. Nevertheless, not every issue brought out by the stakeholders was addressed with matching suggestions for how they could
Greater financing
In particular, CHWs indicated that receiving remuneration for attending supervisory sessions would serve as a source of motivation, highlighting increased financing for supervisory purposes as a crucial aspect. Since many female CHWs also served as moms, this seemed to be especially crucial for them. Receiving requests for monitoring presents another difficulty. For instance, I am in no way assisted in leaving my house while I am a breastfeeding mother, nor are there any other people like me. It would be really beneficial if they could inspire the few VHTs (CHWs) among us, as we really do face all kinds of challenges whether or not we receive financial assistance. (Female VHT)
Structure and design changes to supervisory
The significance of drafting defined job descriptions—which have to include supervisory duties—was also emphasized by DHO stakeholders. They also recommended that special training be provided to those appointed to supervisory roles and that oversight be conducted to guarantee that supervision was taking place. Then assign the task of supervision to the person whose job description it is. Since I will then ask you to serve as your supervisor throughout my evaluation of you Why didn’t you produce this much? You were the one in charge of these VHTs (CHWs). Describe the benefits that resulted from the supervision. (District Official). But we must also get together. Learn how the VHT [CHW] can function and communicate with the responsible supervisor. Talk to them and find out if the community’s problems that the VHTs have identified are being addressed. (District Official)
In addition, CHWs recommended streamlining procedures by having supervisory meetings held at the village level instead of the health center, conducting remote supervision via cell phones, holding more frequent supervision sessions, and having supervisors proactively address issues and difficulties they encountered. The supervisors ought to pay us a visit in our villages. (Female VHT) Communication is also made easier by mobile phones. For instance, you could give your boss a quick call and ask them a question. (Male VHT).
DISCUSSION
The results of this exploratory mixed-methods study show that volunteer VHT supervision is provided in an unorganized and fragmented manner within a single area in Uganda’s Mitooma District. Given that the 341 VHTs could not agree on a single aspect of how supervision is currently provided, it is evident that the current model of supervision is inconsistent. Though most VHTs in this study concurred that supervision took place every three months, there was greater variation in their views regarding the nature and manner of supervision as well as the supervisor’s perceived authority. This result is consistent with earlier research from other LMICs, indicating that CHW supervision is frequently executed inadequately and emphasizing the necessity of paying more attention to the planning and execution of supervisory initiatives. An additional significant discovery pertained to the disparate conceptualizations of supervision. Although all parties involved believed that supervision may help VHTs become more motivated, the VHTs themselves saw supervision as a tool to keep an eye on their work in a management capacity. The positive components of management supervision, which center on task performance and accountability, must, however, avoid veering into control and fault finding, since this could sour relations between VHTs and their supervisors.
While supportive supervision has become more popular in the literature (9), it won’t be easy to put this into reality because of how deeply ingrained people’s perceptions of supervision are. It may be tough to challenge this status quo, and doing so will need extensive consultation with important stakeholders to learn about their perspectives on the best ways to implement supportive supervisory techniques. It is important to consider the hiring and training of supervisors in order to facilitate supportive supervisory practices. This is significant since it has been discovered that one of the primary demotivating issues for CHWs in Ethiopia, Kenya, Malawi, and Mozambique is fault-finding supervisory procedures. (29). It is possible for other nations to emulate Ghana’s recent development of guidelines for CHW supervisor training by government and NGO partners. Developing leadership abilities, giving constructive feedback, and actively listening are just a few of the communication skills that supervisors can improve by following these principles (30). The CHW stakeholders that we interviewed for our study likewise recommended the importance of these elements. Given that prior research has shown that improved sentiments of trust and support between the supervisor and supervisee can lead to better levels of CHW performance, it is worthwhile for supervisors to develop their interpersonal skills (29).
The financial obstacles that prevented individual CHWs from attending centralized supervision sessions were also a source of logistical issues when it came to sponsoring supervisory activities. It is believed that maintaining CHW motivation and ensuring that programs run smoothly depend on the equitable and continuous remuneration of CHWs (31). To enhance the influence of Community Health Workers (CHWs) in their communities, a prior study conducted in Uganda showed that providing financial incentives together with supportive monitoring was beneficial (32). In the Arua District, for instance, the number of malnourished children admitted to intervention institutions increased when CHWs got remuneration (32). The way supervision is now organized and provided, according to CHWs, is another obstacle to it. CHWs suggested that village-level monitoring should take place in place of a type of supervision that involves sporadic meetings in classrooms or at key gathering places. By using this method, supervisory encounters might center on real-world scenarios that CHWs confront on a regular basis, and program design and delivery could become more sensitive to the needs of CHWs. Utilizing mobile technologies (mHealth) to facilitate remote supervision was one of the other recommendations.
Recasting oversight as a continuous process as opposed to a one-time occurrence could be aided by such an approach. Although mHealth techniques shouldn’t be seen as a magic bullet for handling the difficulties of supervision, nor should they take the place of excellent in-person supervision, they might be used as a supplement to make in-person supervision easier in this situation. The problem of having few supervisors, which is a rate-limiting step for the quantity of in-person supervision that may occur, makes this especially crucial in LMIC settings. In Kenya, for instance (33) reported on the ways in which the use of WhatsApp, a mobile instant messaging software, aided in the supervision of 41 CHWs and facilitated communication, information sharing, and the development of a good atmosphere.
CONCLUSIONS
UHC’s fundamental tenet is the caliber of its medical care. In order to do this, the majority of LIC’s lack of human resources for health and other systemic issues highlights the necessity of supportive supervision. To fully realize the benefits of an intervention, it is necessary to address the gaps in current knowledge regarding what makes for good supervision and the necessity of comprehending how various approaches affect performance in various social and cultural contexts. In order to lessen the systemic and logistical obstacles that impede implementation, it is therefore helpful to promote a shared understanding of the concept and a methodological shift that increases capacity at the lower levels of service delivery for internal supporting monitoring, particularly in health facilities. In many LICs, the routine external supervisor model and the financial and logistical needs that go along with it are unsustainable. The importance of task assistance, human connections based on trust, secrecy, and empathy, and the quality of supportive supervision over frequency are all critical.
REFERENCES
- Exploring supervision for volunteer community health workers in Mukono District, Uganda: An,exploratory mixed-methods study. James O’Donovan, Allan Saul Namanda & Rebecca Hamala: Global Public Health, 2021. https://doi.org/10.1080/17441692.2021.1969671.
- Community health volunteers could help improve access to and use of essential health services by communities in LMICs: An umbrella review. MirkuzieWoldie, Garumma Tolu Feyissa, Bitiya Admasu, Kalkidan Hassen, Kirstin Mitchell, Susannah Mayhew, Martin McKee, and Dina Balabanova: Health Policy and Planning, 2018. https://www.researchgate.net/publication/330010000.
- Practitioner Expertise to Optimize Community Health Systems: Harnessing Operational Insight. Madeleine Ballard, Ryan Schwarz, Daniel Palazuelos, English G Sall: Research Gate, 2017. https://www.researchgate.net/publication/321214428.
- Moving to a strong(er) community health system: analysing the role of community health volunteers in the new national community health strategy in Malawi. Vibian Angwenyi, Carolien Aantjes, Ketwin Kondowe, Joseph Zulu Mutchiyeni, Murphy Kajumi, Bart Criel, Jeffrey V Lazarus, Tim Quinlan, Joske Bunders-Aelen: BMJ Glob Health, 2018. 2018;3:e000996. doi:10.1136/bmjgh-2018-000996.
- Community Health Workers in Low-, M Community Health Workers in Low-, Middle-, and High-Income Countries: An Overview of Their History, Recent Evolution, and Current Effectiveness. Henry B. Perry, Rose Zulliger, and Michael M. Rogers: Annu. Rev. Public Health, 2014. publhealth.annualreviews.org.
- Setting the global research agenda forcommunity health systems: literature and consultative review. Smisha Agarwal, Karen Kirk, Pooja Sripad, Ben Bellows, Timothy Abuya and Charlotte Warren: Human Resources for Health, 2019. https://doi.org/10.1186/s12960-019-0362-8.
- From Community Health Workers to Community Health Systems: Time to Widen the Horizon? Lehmann, Helen Schneider & Uta: Health Systems & Reform, 2016. DOI: 10.1080/23288604.2016.1166307 https://doi.org/10.1080/23288604.2016.1166307.
- Potential challenges of implementing the Community Health Extension Worker programme in Uganda. James O’Donovan, Christina Elise Stiles, Deogratias Sekimpi, Isaac Ddumba, Niall Winters, Edward O’Neil Jr: BMJ Glob Health, 2018. 2018;3:e000960. doi:10.1136/bmjgh-2018-000960.
- Supportive supervision to improve service delivery in low-income countries: is there a conceptual problem or a strategy problem? Gertrude Sika Avortri, Joy Belinda Nabukalu, Juliet Nabyonga-Orem: BMJ Glob Health, 2018. 2019;4:e001151. doi:10.1136/bmjgh-2018-001151.
- Village Health Team Functionality in Uganda: Implications for Community System Effectiveness. Babughirana Geoffrey, Muhirwe Barungi Lorna, Kimurahebwe Clare: Science Journal of Public Health, 2016. http://www.sciencepublishinggroup.com/j/sjph doi: 10.11648/j.sjph.20160402.16 .
- Supporting and retaining Village Health Teams: an assessment of a community health worker program in two Ugandan districts. Daniel C. Mays, Edward J. O’Neil Jr, Edison A. Mworozi, Benjamin J. Lough, Zachary J. Tabb, Ashlyn E. Whitlock, Edward M. Mutimba, and Zohray M. Talib: International Journal for Equity in Health, 2017. DOI 10.1186/s12939-017-0619-6.
- Challenges to hypertension and diabetes management in rural Uganda: a qualitative study with patients, village health team members, and health care professionals. Haeyoon Chang, Nicola L. Hawley, Robert Kalyesubula, Trishul Siddharthan, William Checkley, Felix Knauf and Tracy L. Rabin: International Journal for Equity in Health, 2019. https://doi.org/10.1186/s12939-019-0934-1.
- Who is a community health worker? – a systematic review of definitions. Abimbola Olaniran, Helen Smith, Regine Unkels, Sarah Bar-Zeev and Nynke van den Broek: Global Health in Action, 2017, Vol. 10. http://dx.doi.org/10.1080/16549716.2017.1272223.
- Cases in Global Health Delivery: Community Health Workers. Hospital, Havard Medical School and Brigharm and Women’s. 2018.
- Health policy and system support to optimise community health worker programmes: an abridged WHO guideline. Giorgio Cometto, Nathan Ford, Jerome Pfaffman-Zambruni, Elie A Akl, Uta Lehmann, Barbara McPake Madeleine Ballard, Maryse Kok Maisam Najafizada, Abimbola Olaniran, Onyema Ajuebor, Henry B Perry, Kerry Scott, Bianca Albers, Aron Shlonsky, David Taylor: Health Policy, 2018. http://dx.doi.org/10.1016/S2214-109X(18)30482-0.
- Analysis and use of community-based health service data; Guidance for Community Health Workers Strategic Information and Service Monitoring. United Nations Children’s Fund, World Health Organization, Global Fund to Fight AIDS, Tuberculosis and Malaria, United Nations Entity for Gender Equality and the Empowerment of Women, and Gavi, the Vaccine Alliance: United Nations Children’s Fund (UNICEF), 2021.
- Supportive supervision to improve service delivery in low-income countries: is there a conceptual problem or a strategy problem? Gertrude Sika Avortri, Joy Belinda Nabukalu, Juliet Nabyonga-Orem: BMJ Glob Health, 2018. 2019;4:e001151. doi:10.1136/bmjgh-2018-001151.
- Association between supportive supervision and performance of community health workers in India: a longitudinal multi‑level analysis. Lakshmi Gopalakrishnan, Nadia Diamond‑Smith, Rasmi Avula, Purnima Menon, Lia Fernald, Dilys Walker and Sumeet Patil: Human Resources for Health, 2021. (2021) 19:145https://doi.org/10.1186/s12960-021-00689-7.
- Making Supervision Supportive and Sustainable: New Approaches to Old Problems. Lani Marquez, Linda Kean: USAID, 2002. Sciences for Health under USAID cooperative agreement HRN-A-00-00-00014-00.
- National guidance and district-level practices in the supervision of community health workers in South Africa: a qualitative study. Schneider, Tumelo Assegaai and Helen: Human Resources for Health, 2019. https://doi.org/10.1186/s12960-019-0360-x.
- Supportive supervision and constructive relationships with healthcare workers support CHW performance: Use of a qualitative framework to evaluate CHW programming in Uganda. Teralynn Ludwick, Eleanor Turyakira, Teddy Kyomuhangi, Kimberly Manalili, Sheila Robinson, and Jennifer L. Brenner: Human Resources for Health, 2018. (2018) 16:11https://doi.org/10.1186/s12960-018-0272-1.
- The status of Ghanaian community health workers’ supervision and service delivery; descriptive analyses from the 2017 Performance Monitoring and Accountability 2020 survey. Dan Schwarz, June-Ho Kim, Hannah Ratcliffe, Griffith Bell, John Koku Awoonor-Williams, Belinda Nimako, Easmon Otupiri, Stuart Lipsitz, Lisa Hirschhorn, Asaf Bitton: Gates Open Research, 2019. https://doi.org/10.12688/gatesopenres.12979.3.
- How to create more supportive supervision for primary healthcare: lessons from Ngamiland district of Botswana: co-operative inquiry group. Oathokwa Nkomazana, Robert Mash, Silvia Wojczewski, Ruth Kutalek and Nthabiseng Phaladze: Global Health Action, 2016.
- National Population and Housing Census 2014: Area Specific Profiles Mitooma District. UBOS: UBOS, 2017.
- Uganda Demographic and Health Survey. Statistics, UBOS: Uganda Bureau of Statistics, Kampala Uganda, 2016.
- Performance of community health workers and associated factors in a rural community in Wakiso district, Uganda. Musoke, Rawlance Ndejjo, Edwinah Atusingwize, Trasias Mukama, Charles Ssemugabo, Linda Gibson: Afri. Health Sci., 2019. 2019;19(3): 2784-2797. https://dx.doi.org/10.4314/ahs.v19i3.55.
- Impact Report. Action for Community Development: ACODEV, 2022.
- The impact of a supportive supervision intervention on health workers in Niassa, Mozambique: a cluster-controlled trial. Tavares Madede, Mohsin Sidat, Eilish McAuliffe, Sergio Rogues Patricio, Ogenna Uduma, Marie Galligan, Susan Bradley and Isabel Cambe: Human Resources for Health, 2017. DOI 10.1186/s12960-017-0213-4.
- Optimising the benefits of community healthworkers’ unique position between communities and the health sector: A comparative analysis of factors shaping relationships in four countries. Maryse C. Kok, Hermen Ormel, Jacqueline E. W. Broerse, Sumit Kane, Ireen Namakhoma, Lilian Otiso, Moshin Sidat, Aschenaki Z. Kea, Miriam Taegtmeyer, Sally Theobald & Marjolein Dieleman: Global Public Health, 2017. https://doi.org/10.1080/17441692.2016.1174722.
- Ghana National Community Health Worker Training Manual. Republic of Ghana Ministry of Health: World Vision International and Ghana Ministry of Health/Ghana Health Service, 2015.
- Salaried and voluntary community health workers: exploring how incentives and expectation gaps influence motivation. Hermen Ormel, Maryse Kok, Sumit Kane, Rukhsana Ahmed, Kingsley Chikaphupha, Sabina Faiz Rashid, Daniel Gemechu, Lilian Otiso, Mohsin Sidat, Sally Theobald, Miriam Taegtmeyer and Korrie de Koning: Human Resources for Health, 2019. https://doi.org/10.1186/s12960-019-0387-z.
- Supportive supervision to improve the quality and outcome of outpatient care among malnourished children: a cluster randomised trial in Arua district, Uganda. Marzia Lazzerini, Humphrey Wanzira, Peter Lochoro, Richard Muyinda, Giulia Segafredo, Henry Wamani, Giovanni Putoto: BMJ Global Health, 2019. 2019;4:e001339. doi:10.1136/bmjgh-2018-001339.
- Enhancing the Supervision of Community Health Workers With WhatsApp Mobile Messaging: Qualitative FindingsFrom 2 Low-Resource Settings in Kenya. Jade Vu Henry, a Jade Vu Henry, Niall Winters, Alice Lakati, Martin Oliver, Anne Geniets, Simon M Mbae, Hannah Wanjiru: Global Health: Science and Practice, 2016.

