‘Abstinence-Be-Faithful-Condom-use’ model of HIV/AIDS preventive knowledge and practices in Lower Manya Krobo Municipality in Ghana
- Adjoa Afriyie Poku
- 1028-1046
- Apr 18, 2023
- Public Health
‘Abstinence-Be-Faithful-Condom-use’ model of HIV/AIDS preventive knowledge and practices in Lower Manya Krobo Municipality in Ghana
Adjoa Afriyie Poku
Department of Geography Education, Faculty of Social Science, University of Education, Winneba, Ghana
Received: 20 February 2023; Revised: 15 March 2023; Accepted: 21 March 2023; Published: 18 April 2023
ABSTRACT
The study examined the ‘Abstinence-Be-Faithful-Condom-use (ABC) model’ of HIV/AIDS preventive knowledge and practices among rural and urban residents in Lower Manya Krobo Municipality (LMKM). The study adopted a cross-sectional survey under the descriptive study design. Systematic and purposive techniques were used to sample 362 respondents, and 52 participants. Questionnaire and unstructured interview were used to gather data from the respondents and participants in the LMKM. Descriptive statistics and thematic analysis were used to analyse quantitative and qualitative data obtained for the study. The study revealed that urban dwellers have good knowledge of and practised the ‘ABC’ model of HIV prevention compared to rural dwellers in the LMKM. Urban dwellers have good knowledge on abstinence as a preventive measure of HIV compared to rural dwellers. The study also found that, both rural and urban dwellers practised faithfulness, however, both rural and urban dwellers misunderstood the term being faithful as they had more lifetime sexual partners which does not conform to the ‘ABC’ model. Rural dwellers exhibited low knowledge and use of condoms compared with urban dwellers. It is therefore recommended that there should be a collaboration between the Municipal Health Directorate, Ghana AIDS Commission, country office of the World Health Organization, National Commission on Civic Education, community leaders and non-governmental organizations to expedite action on educating the communities on HIV preventive practices in the municipality focusing more on rural communities.
Keywords: Abstinence, Faithful, Condom, HIV/AIDS, preventive knowledge, practices, Lower Manya Krobo Municipality, Ghana
INTRODUCTION
In the world at large, the Human Immunodeficiency Virus continues to be one of the most serious public health problems (Quarm et al., 2021). It has been reported that approximately 36.3 million people died from HIV/AIDS in 2021, and there were 37.7 million HIV-positive people globally as of the end of 2020, with more than two-thirds of those people living in Sub-Saharan Africa (Cherie et al., 2022). To minimise the spread of the disease, the “ABC” model of HIV prevention practice, where A stands for abstinence or delay of sexual activity, B for be faithful, and C for condom use, (Shelton et al., 2004) and also early HIV detection and prevention gives hope for Africans in the sub-region. Though these are preventive measures for acquiring HIV, they are however not known to everyone. People infected with HIV can go years without showing any symptoms, making it possible for people with the virus to be unaware of their condition and infect others (Jennifer et al., 2010). Additional information to this reveals that South Africa, which is one of the HIV-prone countries has only 14.4% of the population who are aware of some symptoms of HIV infection (Zuma, et al., 2022). Due to inter-regional movement, immediate action is needed to promote HIV intervention programmes in South Africa to save a large number of the population and the Sub-Saharan region as a whole.
HIV/AIDS is one of the illnesses that have an impact on patients’ social and psychological well-being in addition to their physical health (Kose et al., 2012). People with this disease may experience a wide range of issues in addition to the physiological effects of the disease, including discrimination, loss of social status and role, changes in intimate relationship patterns, job loss, a lack of financial resources, and difficulty obtaining the necessary medications (Dejman et al., 2015). Though the ABC model of HIV preventive practice is the best-known strategy to minimise the transmission of HIV (Bell, 2014), young individuals are anticipated to harbour around a third of all new infections globally, and are particularly at risk of this challenge since the proportion of people infected with HIV who are aware of their status is thought to be much lower (Safeek et al., 2018). This creates a serious public health issue as it was discovered that about 50% of young persons with HIV are not identified and treated to decrease their viral loads (Koenig et al., 2016; Safeek et al., 2018).
History of HIV/AIDS in Ghana has it that prior to the first AIDS case being announced in 1986, the PNDC government took action to lessen the effects of the HIV/AIDS epidemic (Halasa-Rappel et al., 2021). These actions included the commitment to controlling the disease and implementing measures such as HIV/AIDS awareness campaigns in schools and amending laws and regulations to safeguard those who were most at risk of contracting it (Halasa-Rappel et al., 2021). Due to the looming economic woes of the government, there was inadequate funds to continue the HIV intervention programmes. This is the reason Integrated Regional Information Networks (United Nations)has reported that the Ghanaian government’s AIDS programme is at risk of failing, partly because of stigma and a poor health system (Ghana AIDS Commission, 2014) arising from inadequate funds. This has led to a gradual increase in the HIV infection rate in the country, which in a long run, made Lower Manya Krobo Municipality have a higher HIV infection rate among the districts in the country (Ofori et al., 2022).
Lower Manya Krobo Municipality (LMKM) is one of the districts in the Eastern Region of Ghana. This municipality has the highest HIV/AIDS prevalence and statistically, highest infection rate in the country at 5.6%, compared to the country’s overall average of 2.66% in 2018 (Ghana AIDS Commission, 2019; Ofori et al., 2022). It is also quite surprising that the majority of the people of LMKM have relatively low knowledge of the mode of HIV transmission and prevention practices in the municipality as it has been recommended that community opinion leaders and stakeholders sensitize community members to better understand the HIV transmission modes and preventive practices (Owusu & Laar, 2018).
Preventive knowledge and practices of HIV are necessary for people to lower their risk of contracting the infection, particularly by abstinence (A), faithfulness to one partner (B), the use of condoms during sexual intercourse (C), models and to some extent, early HIV detection, treatment and prevention (Marrazzo & Cates, 2011; Workowski & Bolan, 2015). However, a study has shown that not all people in Lower Manya Krobo Municipality are willing to test to know their status (Apanga, et al., 2015).Studies on this municipality in relation to HIV transmission have focused on the cultural sustainability of the dipo rite (Poku, 2022), conflicting sex education policies (Ocran, 2022), and gendered analysis (Owusu, 2020). More so, considering the ABC model for preventing the transmission of HIV, it is important to understand the knowledge and preventive practices regarding HIV among rural and urban dwellers as a study has shown that HIV/AIDS is more prevalent among rural dwellers (Appiah et al., 2022). It is against this background that this study sought to examine the ‘Abstinence-Be-Faithful-Condom-use (ABC) model’ of HIV/AIDS preventive knowledge and practices among rural and urban residents in Lower Manya Krobo Municipality in Ghana, West Africa.
The study’s findings could serve as the basis for organizing sensitization programmes targeted at preventing and controlling the spread of HIV/AIDS among rural and urban dwellers in the municipality. More so, researchers, local and national health officials, and organizations such as the Ghana AIDS Commission, and the Centre for Disease Control and Prevention could benefit from this study as this research could inform their planning, monitoring and implementation strategies regarding the prevention and control of the HIV infection in Ghana.
METHODS
Study area
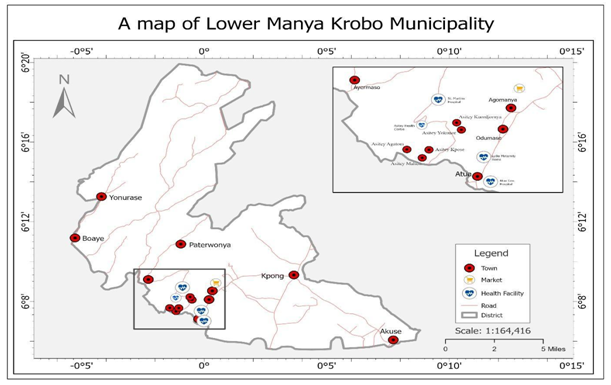
The study was conducted in the Lower Manya Krobo Municipality (LMKM) in the Eastern Region of Ghana. The municipality lies between latitudes 6º05N and 6º30N and longitudes 0⁰08W and 0º20W. The LMKM shares boundaries with the Upper Manya Krobo District at the North West, the Asuogyaman District in the northeast, North Tongu District in the south eastern and the Yilo and Dangme West in the south (See Figure 1) (Poku, 2022).
Figure 1: Study area (LMKM).
Source: Danso, 2023
The municipality covers a total land area of 591 sq. km which is only 3.21 percent of the total land area of the Eastern Region which is 18,310 km (Lower Manya Krobo Municipal Assembly, 2022).The 2021 population and housing census indicated a population size of 121, 478 with a higher female population (53.4%) than males (46.6%) (GSS, 2021). The population of the municipality is unevenly distributed as major settlements are strategically located in a nucleated form but linearly along the only trunk road from Accra to Akosombo. The major economic activity in the area is agriculture which currently employs about 80% of the people in the municipality (LMKM Profile, 2020). The municipality has four Reproductive and Child Health Centres (RCHC), in the township of Akuse, Kpong, Asitey and Oborpa sub-districts; nine Community-Based Health Planning Services (CHPS) zones; and two government hospitals in Atua and Akuse; and one mission hospital in Agormanya, 9 traditional birth attendants, traditional healers, licensed chemical sellers and 59 community-based volunteers (LMKM Profile, 2020). Several rural areas in Ghana have in recent times recorded an upsurge in HIV prevalence rates. Thus, data from the Ghana Health Service reported that the LMKM area in the Eastern Region of Ghana has persistently recorded very high HIV and AIDS prevalence rates and AIDS deaths from 1998 to 2000, 2014 to 2020. LMKM is thus, not the only rural sites in Ghana faced with a high prevalence of HIV cases and AIDS death (NACP & GHS, 2020). The municipality was purposely selected based on the reported cases of high incidence of HIV and AIDS deaths to ascertain the ‘ABC’ model of HIV/AIDS preventive knowledge and practices in LMKM in Ghana.
Study design
The study used cross-sectional survey under descriptive research design. This design is used to describe a population or phenomenon. It was used to systematically obtain information from the respondents using varied methodologies to describe ABC’ model of HIV/AIDS preventive knowledge and practices in LMKM in Ghana using simple percentages without regard to any causal or other hypothesis (Aggarwal & Ranganathan, 2019).This design ensures adequate information from respondents through communication and cooperation between the researcher and the respondents through the use of various methods by the researcher. Cross-sectional survey design is a type of observational study design, which measures the outcome and the exposures in the study participants at the same time. The participants in a cross-sectional study are just selected based on the inclusion and exclusion criteria set for the study (Setia, 2016).
The sample, sampling technique and procedure
This study specifically used both systematic and purposive sampling techniques. The researcher beginning from one end of the town or village systematically sampled every sixth house and women and men aged 15 years and above were selected.The purposive sampling techniques was used to select key informants who had in-depth knowledge about the issue and were willing to participate in this study. The views of respondents totaling 362 (306 in the urban community and 56 in the rural community) and 52 participants viz; health officials (n=13), municipal and local leaders (n=7), religious leaders (n=7), drug store owners (n=3) and local residents (n=22) in the LMKM were sought.
Data generation and ethical consideration
A questionnaire and unstructured interview were used to gather data from the respondents. The questionnaire was for the respondents while the unstructured interviews were conducted with the participants. Both categories of the sample we initially approached and informed of the purpose of the study. The objectives of the study were further explained to those who were willing to take part in the study. Verbal consent was then sought from each respondent and participant before questionnaires were administered and interviews conducted. The questionnaire was used to gather data from respondents in Agormanya (Urban) and Asitey (Rural) while the interview guide was used to collect data from key participants. Agormanya and Asitey were selected for the study because they had the highest population within the urban and rural categories and have health facilities that serve towns and villages in the area and provide services in the form of Voluntary Counselling and Testing (VCT) and treatment for HIV/AIDS patients in the municipality.
The questionnaires were filled out immediately in the presence of the researcher and taken. Questions on the questionnaire were read out and translated into the local dialect of the respondents who could not read the English language. In-depth interviews were also conducted with participants in the location where the person was recruited, which was mostly the subject’s private offices and homes. Interviews were conducted in a secure environment free from third-party interference. With regards to the health officials, the interviews were conducted in their separate unused consulting rooms after their regular daily activities. The municipal and local leaders were also interviewed at their offices at the palace whilst the religious leaders were interviewed at their shrines and church premises without any interference. The drug store owners were also interviewed at their shops while interviews for ordinary residents were conducted in their homes.
Interviews were conducted in Ga Adangme (the local dialect) of the two communities, with Akan and English Language to serve the needs of the participants with different socio-economic and literacy levels. The instruments were developed based on questions relating to the views of the respondents on ‘ABC’ model of HIV/AIDS preventive knowledge and practices in LMKM in Ghana. Interviews were audio recorded after participants consented. This helped to record the participants’ responses verbatim. Field notes were also taken. The audio records were transcribed into English. Each interview lasted for approximately 40 minutes. To ensure ethical consideration, anonymity and confidentiality were ensured. No names were assigned to any data collected. Also, the Ethics Committee of the St Martins de Porres Hospital in LMKM provided ethical approval for this study.
Data analysis
Data derived from the questionnaire was coded into the SPSS version 24. Descriptive statistics was used to analyse the data in addition to thematic analysis. This was presented in the form of percentages. The views of the participants were summarized and coded based on themes. Initially, open coding of the data was done. These generated a series of themes after thorough multiple readings of the transcripts. The themes were compared with the responses to identify common trends, similarities and differences. Thematic analysis enabled the researcher to summarize key features of the large data set and take a well-structured approach to handling data, and helping to produce a clear and organized data in full details (King, 2004).
RESULTS AND DISCUSSION
The socio-demographic characteristics distribution of rural and urban respondents is presented in Table 1. Females constituted the majority in both rural (60%) and urban (61.6%). All except 16.0% and 8.5% of rural and urban respondents respectively had some formal education. 17.9% of rural respondents and 34.0% of urban respondents had secondary and higher education. This shows that the respondents can understand the ‘ABC’ model of HIV preventive measures. Marital status distribution showed that while 34.6% of urban respondents were single, 39.2% each of rural respondents were either married or single.
Table 1: Socio-demographic characteristics of respondents
| Variable | Responses | Percentage |
| Sex | ||
| Rural | ||
| Male | 19 | 40.0 |
| Female | 37 | 60.0 |
| Total | 56 | 100.0 |
| Urban | ||
| Male | 118 | 38 |
| Female | 18 | 61.4 |
| Total | 306 | 100 |
| Educational level
Rural |
||
| No formal | 9 | 16.0 |
| Basic | 37 | 66.0 |
| Secondary/Higher | 10 | 17.9 |
| Total | 56 | 100 |
| Urban | ||
| No formal | 26 | 8.5 |
| Basic | 176 | 57.5 |
| Secondary/Higher | 104 | 34.0 |
| Total | 306 | 100.0 |
| Marital status
Rural |
||
| Single | 22 | 39.2 |
| Living with a partner | 10 | 17.8 |
| Married | 22 | 39.2 |
| Widowed | – | – |
| Divorced | 2 | 3.5 |
| Total | 56 | 100 |
| Urban | ||
| Single | 106 | 34.6 |
| Living with a partner | 69 | 22.5 |
| Married | 103 | 33.6 |
| Widowed | 18 | 5.8 |
| Divorced | 10 | 3.3 |
| Total | 306 | 100.0 |
Source: Field work, 2022
Out of the 13 health officials interviewed four (4) possessed Bachelor’s degree in Medicine and 9 nurses had Diploma in General Nursing. One (1) municipal and local leader possessed a Bachelor’s degree in Planning while the remaining 6 possessed Diploma certificates. Five (5) of the religious leaders had Diploma in Theology while 2 of them had one-year certificates. All the three (3) drug store owners had attained secondary/higher education, while 16 of the local residents had basic education, 2 had no formal education and 4 had secondary/higher education.
‘ABC model’ of HIV prevention knowledge and practices in LMKM
Respondents and participants view on ‘ABC’ model of HIV/AIDS preventive knowledge and practices in LMKM were sought, assessed and analysed under the following themes; Abstinence, Be faithful and other knowledge on HIV preventive measures and knowledge on condoms as HIV preventive measure in LMKM.
Abstinence, Be faithful and other knowledge on HIV preventive measures in the LMKM
Various researchers including Campbell (1997) and Teye (2004) have asserted that health related behaviour is determined by an individual’s knowledge level of a disease including preventive measures. The study asked questions to find out respondents and participants knowledge and practice of the Abstinence component of the ‘ABC model’. The findings from the interview revealed that abstinence was found to be one of HIV prevention measures used in LMKM. This limits the chances of people contracting HIV. A participant said:
“For me I do not have sex at all so that I will not catch the virus.”(Rural resident 2)
Quantitative data to find out their knowledge on abstinence as HIV preventive measure on the contrary revealed that a majority of the rural dwellers (53.5%) disagreed that abstaining from sex is HIV preventive practice while 67.5% of urban dwellers agreed. Abstinence has been one strategy that has contributed to the reduction in HIV infection rate among the current youth in developing countries like Ghana. This demonstrates discipline and faithfulness in a sexual relationship as a form of HIV preventive measure (Zulu et al., 2002). On the contrary, it is usual for people with less knowledge on HIV prevention to assume that the virus can only be transmitted to another individual through sexual intercourse and thus, practise abstinence.
Moreso, the study asked questions to find out respondents and participants knowledge and practice of the Be faithful component of the ‘ABC model’. The study revealed that participants and respondents were maintaining one partner at a time. Some of the interview participants explained further as demonstrated in the following quotations:
“I am protecting myself from HIV. For me, I maintain one partner at a time. I don’t keep two or more partners at a time. If I end with one before I go for another so I am faithful to the one I am with. It is good to stay with one partner and not patronising prostitutes you will not catch the disease.” (Urban resident 1)
“I keep one girlfriend at a time and when I stop with her before I go for a new girl so I don’t think I will get AIDS…..I believe I am safe” (Rural resident 1)
Although, sticking to one partner has been a common measure to curb the spread of HIV among individuals and communities, it is evident from the quotations that most of the participants have had more lifetime sexual partners. The interviews further revealed that a majority of them have had more than 5 partners suggesting that they engaged in ‘serial monogamous relationships. This kind of phenomenon is not limited to one participant; as it is a common practice for young people in the municipality to stay in sexual relationships with one partner for a while and end the relationship to begin a new one. This is contrary to the ‘be faithful’ in the ‘ABC’ model which stipulates that people should have fewer lifetime sexual partners and encourages individuals to practice fidelity in marriage and other sexual relationships as a critical way to reduce risk of exposure to HIV and thus, once a person begins to have sex, the fewer lifetime sexual partners he or she has, the lower the risk of contracting HIV (Shelton et al., 2004).
However, when respondents were asked whether limiting sex or staying faithful to one partner prevents HIV in the municipality, there were mixed responses as a majority (64%) of rural respondents did not respond to the question. This may be because more of the rural dwellers tolerated multiple sexual relationships and therefore were silent about it. This explains the assertion that a section of rural dwellers was more likely to engage in multiple sexual relations as compared to urban dwellers (Chae & Agadjanian, 2022). However, less than half (32.1%) of rural respondents and almost all (97.0%) of the urban respondents agreed that limiting sex or staying faithful to one partner reduces a person’s risk of contracting HIV/AIDS. This is in line with a study conducted in some highly infected HIV countries in Sub-Saharan Africa that more urban dwellers show a higher knowledge of HIV infection (Wang et al., 2012) and this may include faithfulness to one partner as a preventive measure to contracting the HIV infection.
Participants and respondents were asked questions on other HIV preventive practices in LMKM. Responses on whether refusal to take blood transfusion is an HIV preventive measure revealed that a majority of both rural (75.0%) and urban (65.9%) respondents disagreed that refusal to take blood transfusion is an HIV preventive measure and rather taking blood transfusion from the hospitals are safe and could not transmit the virus. This was further supported by views of some residents who took part in the interview as expressed in the comments:
“I don’t think the blood that you are given in the hospital do not have HIV. If it has the virus the doctors won’t give it to anyone.” (Urban resident 2)
“The blood that is transfused in the health centre here do not contain HIV. I think they check it before they give it to people who are sick and need it.” (Rural resident 3)
The above response indicated that the study participants were very aware that HIV can be transmitted through blood and blood products but they were also aware that before blood is transfused to a different person in hospitals it is screened to check for infections including HIV and hepatitis B. Interviews with health officials further reported that blood for the blood banks in the hospitals are screened before being used. This suggested that health facilities in the area follow WHO policy on safe medical procedures. Notwithstanding this, a study on HIV transmission has shown that compared to sexual transmission, HIV transmission through blood-to-blood contact or blood transfusion is quite higher (Patel et al., 2014), questioning the knowledge of the respondents and participants on HIV transmission and prevention practices.
The study asked a question on whether avoiding sex with commercial sex workers is an HIV preventive measure. A majority of respondents (83.9%) in the rural areas and (98.4%) in the urban areas agreed that avoiding sex with commercial sex workers reduces a person’s risk of contracting HIV infection. This was explained further by some of the participants in the statements:
“I know that most of the woman who are brought back to the village here sick with HIV engaged in prostitution in the cities and return home after contracting the virus. So, if you patronise prostitutes, you will catch the disease.” (Rural resident 5)
“Yes, one may get infected with HIV when you go for prostitutes. I think it is good for us not to have sex with commercial workers.” (Urban resident 4)
Research have shown that HIV prevalence is high among marginalized groups such as gays, people who inject drugs, and sex workers (Smith et al., 2009). Therefore, the responses above conforms to what a study has revealed that lowering sex works reduces the risk of contracting the HIV infection (Deering et al., 2013; Platt et al., 2018).
Also, the study solicited information from the respondents on whether kissing could prevent HIV transmission in LMKM. It was found that a majority (60.7%) of rural respondents disagreed that kissing could result in HIV transmission while majority (57.7%) of their urban counterparts were of the opinion that kissing could result in HIV infection.
“I don’t think you may get the disease when you kiss someone.” (Rural resident 6)
“One may get the disease if you kiss some having sore in the mouth. In most cases blood may come out of the person’s mouth.” (Urban resident 5)
Though kissing, specifically, deep kissing is an affectionate way of communicating sexual love between partners, saliva which ends up in the buccal cavity after this practice is thought to have possible viruses such as HIV from the infected person (Touyz & Touyz, 2020). The exchange of infected saliva from this practice can lead to the transmission of HIV.
On the question of whether avoiding sharp objects is an HIV preventive measure, the responses revealed that a majority (85.7%) of rural and almost all (96.4%) urban respondents agreed that avoiding sharp objects could prevent or avoid the risk of HIV infection. This finding indicates that knowledge of other various behavioural risk factors for HIV is high in the area. A higher percentage of respondents both in the rural (85.7%) and urban (87.7%) area however, disagreed that injections could result in HIV transmission. In-depth interviews with health officials revealed that new directives from Ghana Health Service (GHS) request that new syringes and needles be used on each patient in almost all the hospitals and health centres throughout the country and this was being adhered to in LMKM. Some participants, however, indicated that one can contract HIV through injections given outside health facilities such as the drug store. Some participants explained that drug store operators sometimes use one syringe to inject many people in order to save cost. This is what one urban resident said:
“Sometimes when I don’t have money to take my child to the hospital, I take him to the drug store for treatment when he is not well. When they have to give him an injection sometimes all that I see is that the drug has been put into the syringe and I don’t know whether it is new or old. When you complain the owner sometimes get offended.” (Urban Resident 6)
It is evident from the statement that although some people may have knowledge on HIV preventive measures, other circumstances including poverty could put people at risk of HIV infection. This drives home the assertion that there is a direct relationship between lower socio-economic status of people and the spread of HIV. This particular finding therefore, has a serious implication for HIV prevention in the municipality.
Knowledge on condoms and its use as HIV preventive measure in LMKM
The study asked questions to find out respondents and participants knowledge and practice of condom use component of the ‘ABC model’. The study asked questions on whether a person could prevent HIV infection by using condoms. The study found a rural-urban differentials in the responses. Thus, half of the rural respondents (52.0%) disagreed that condoms could prevent HIV transmission while (97%) of the urban participants agreed. Interviews conducted supported the findings as expressed in the comments:
“The best way to prevent catching the virus is to use condoms. It is the safest way not to catch the disease.” (Urban resident 3)
“Using condoms cannot prevent HIV spread. I know someone a virgin who has HIV, so what about that. Even if you use condoms, you can get HIV. The condom can even get burst. When you stick to one partner it prevents the disease from spreading” (Rural resident 4)
The narratives brought to bear the perception or knowledge of condom and its potential to cause HIV transmission or prevention. Condom offers three levels of protection: defence against unwanted pregnancy, prevention of the spread of HIV, and other Sexually Transmitted Infections (Stover et al., 2017). Though a number of studies have demonstrated that condoms can prevent the transmission of HIV (Liu et al., 2014; Lasry et al., 2014; Smith et al., 2015), low quality condoms hinder the progress of HIV prevention (Mohammadi Gharehghani et al., 2020), indicating that condoms do not give full protection against HIV to its users.
Respondents were also asked question on whether it is okay to reuse a condom. Majority of respondents in both the rural (62.4%) and urban (82.9%) community disagreed that condoms could be reused. Participants during interview sessions provided explanations:
“I don’t think it is good to reuse condoms. It is used once and you throw it away. If you reuse germs and even the virus can be on it and you can catch it.” (Rural resident 7)
“How can condoms be reused? It’s not possible and its unhygienic to reuse them. It’s not good to even touch them after use.” (Urban resident 7)
There has been misconception on the reuse of condoms as it has been suggested that condom reuse reduces the physical integrity or reliability of the condom (Mbachu et al., 2021) and this can lead to the transmission of HIV. The expression from both the rural and the urban participants suggest that rural and urban dwellers have an appreciable knowledge on condom reuse and its possibility of HIV transmission.
There were differences in responses by residential location with regards to the question on whether condoms protect against diseases. Less than half (43.8%) of the rural respondents agreed while a majority (90.2%) of urban respondents agreed that condoms protect against diseases. Interviews also revealed differences in responses as expressed in the statements:
“Even if you use condoms, you can catch diseases, in fact, the best way is to be careful with one’s life.” (Rural resident 8)
“Yes, when you use condoms, you won’t catch any disease that you can get through sex. For me I think condoms protects against diseases.” (Urban resident 8).
The mistrust for condoms as a form of protection against diseases by the rural participants, as expressed, confirmed the findings that rural dwellers are sceptical of using condoms and that they will rather test for possible infections with their partners before sexual intercourse (Nakiganda et al., 2021).
Respondents were further asked whether a person can get HIV if s/he uses condoms anytime s/he engages in sex. It was found that a majority of the respondents both in the rural (67.9%) and urban (70.5%) agreed that one can get HIV even if the person consistently use condoms in all sexual interactions. Interview participants commented on this question:
“You can still get the virus if you use condoms. Condoms cannot save you from catching the disease it can get burst and you may not know until you finish by then you have gotten the virus.” (Urban resident 9)
“The condom is rubber and the rubber can tear and when it tears you will catch the virus. Witches and demons can also give you the disease so even if you use condoms, you can get the disease.” (Rural resident 9)
It is evident from the statements that, while a good number of urban residents asserted that condoms protect against diseases, they disagreed that condoms use prevent HIV infection effectively. They further reported that, one can contract the virus when condom gets burst. In the case of the rural respondents however, they exhibited low knowledge on condoms with respect to condoms protecting against diseases including HIV infections. Condoms are one of the methods of HIV prevention. However, the use of oil lubricants on condoms and the use of poor-quality condoms may cause the condom to split during sexual intercourse, allowing the flow of infected semen and vaginal fluid into the reproductive organs and causing an HIV infection (Mohammadi Gharehghani et al., 2020; NHS, 2022).
Attitudes and perceptions towards condoms and their use as HIV/AIDS preventive measure in the LMKM
In order to examine the attitudes and perception of respondents towards condoms and their use as HIV/AIDS preventive measure in the LMKM, respondents’ views on use and source of information on condoms, perceptions on condoms and its use and level of educational campaigns on condom use and HIV/AIDS in the municipality were sought.
Use and source of information on condoms
The study sought information from respondents on whether they have ever used a male/female condom. The study revealed a residential differential in the responses. More urban respondents (60%) have ever used condoms than their rural counterparts (25%). This is in line with the study of Ali et al., (2019) that found that the utilization of condoms is more among urban dwellers. These disparities between rural and urban condom use are mostly caused by inequalities between the two in many ways (Hu et al., 2020). As put forward by one study, the disparities are as a result of challenges in the implementation of effective AIDS prevention and intervention services, poor economic conditions, and limited access to healthcare services in the rural areas (Preston et al., 2002).
Moreso, the study asked a question on where respondents get information on condoms. It was revealed that, most of the respondents in both the rural (78.6%) and urban (80.3%) community obtained information on condom from the Radio/TV/Newspapers. Though information on condom use was obtained from Radio/TV/News Papers, other sources of information could be the internet (Mohamad Shakir et al., 2020), peers (Elshiekh et al., 2020) and medical source (Milic et al., 2020). Interviews with Municipal and local leaders and health officials revealed that information on HIV/AIDS and its preventive measures, especially condom use is communicated to the people of the area on the local community radio, through talk shows and advertisements. Most of these talk shows were sponsored by importers of specific brands of condoms who advertise their products and inform the public that they could get their brand of condom at any drug store throughout the country and in the Municipality. Most of the condom importers also sponsored the ‘Ngmayem’ festival of the Krobo people and during the festive period educate the people on the use of condoms while marketing their products. It is obvious from the findings, that through the use of technology, health intervention designers can select the most relevant population for health-related education and programs through the use of conventional communication channels (Nadarzynski, et al., 2019).
The study also asked a question on places where respondents go for condom. The findings revealed that drug store/pharmacy is the place where most of the respondents in both the rural (49%) and urban (85%) community go for condom. However, rural participants (25.0%) were more likely to go for condoms at the health centre compared to their urban counterparts (6.3%). Although, rural participants were likely to go for condoms at the health centre, it was found that condoms were not free from the health centres. One has to buy them but mostly at a cheaper cost as they are either subsidised by government or Non-Governmental Organisations (NGOs). Contrary to what this study found, other studies found that rural dwellers are shy and anticipate scoldness from health professionals at health centres if they are to get condoms (Sychareunetal., 2018). It is added that rural dwellers see the pharmacy as a place of convenient to get condoms (Sychareun et al., 2018) which is not questionable by the pharmacists since the pharmacy is operated as a business venture.
Health official further reported that some of the hospitals in the municipality, in particular, the Catholic Hospital is a mission hospital and, therefore, operates under strict Catholic principles. Interview with one of the health officials at the hospital in the Municipality confirmed this practice:
“This is a Catholic Society so we are against condom use…….we used to have some demonstration on how to use it but we preach abstinence.” (Health Official).
The narrative suggests that the Catholic missionary is against the use of contraceptives in any form and, especially condoms. The Catholic hospital rather preach abstinence and faithfulness and this is confirmed in a statement by one of the health officials at the hospital:
“You are not married but why do you want to have sex……you are still attending school…..” (Health Official)
It is for a fact that some faith-based organizations are against family planning practices including the use of condoms. The expression of the nurse in the narrative above confirms that Catholic health facilities adhere to the policy of abstinence rather than the use of condoms (O’Brien, 2017). More to that, their healthcare professionals are prohibited from recommending or distributing oral contraceptives, and barrier products like condom to clients or patients (O’Brien, 2017).
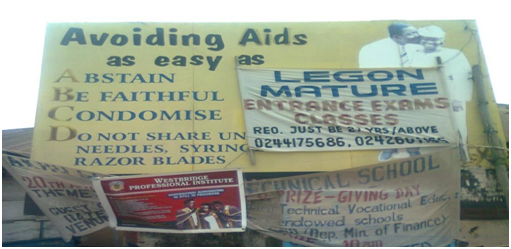
The study also found that HIV/AIDS prevention messages conveyed by health officials at the St Martin Hospital is based only on the A, B, C and D model as shown in Figure 2.
Figure 2: Signboard erected in LMKM to create awareness of HIV/AIDS and its prevention.
Source: Fieldwork, 2022
Information in Figure 2 shows that the ABC model of HIV/AIDS prevention continues to be used in the municipality although messages on stigma prevention, VCT and treatment options are being conveyed alongside in recent times. It is worth noting here that in spite of the interruptions on the advert in the photograph, it is evident that HIV/AIDS awareness education in the area and also in other areas of Ghana place emphasis not only on the three (ABC) behavioural changes model but goes beyond to include a D (do not share unsterilized needles, syringe, razor blade) (Appiah-Agyekum &Suapim, 2013).
Perceptions on condoms and its use in the LMKM
The study sought information on respondents’ perception on condom use. The findings showed residential differentials on perceptions on condom and its use. While less than half of the rural respondents (46.4%) had negative perception on condoms because of problems experienced with its use, more urban respondents (73.4%) exhibited positive perception because they never had problems with its use. Rural participants who had problems with condom use mentioned that condoms got torn in the course of the sexual intercourse. They further complained that the hard texture of some condoms leaves pain in their vagina after sex and, therefore, would not use condoms. Rural female participants also indicated that the use of condom leaves a smell in their vagina which they felt also causes certain infections. Most of the women who took part in the study in both the rural and urban area reported that they had never seen a female condom before and as such had no knowledge on how to use it. This was expressed in the statement by some female participants:
“The first time a man used a condom with me it got burst and we only saw it after we had finished. The male condom can get burst but the female condom looks durable, but it’s not easy getting the female condom at the drug store; using it is complicated. So, I don’t use condoms again.” (Rural residents)
“Some of the male condoms are hard which leaves pains in my private part and because of that I don’t use them anymore. I hear there is a female condom but I don’t know how it looks like.” (Rural residents)
The findings suggest that the common condom used during sexual intercourse is the male condom. It can be concluded from the findings that female condoms receive low patronage(Boakye, 2009) and prove of faithfulness among sexual partners (Ananga et al., 2017).
Additionally, municipal, local and religious leaders indicated that efforts of governments and Non-governmental Organizations in distributing condoms to the youth focus only on male condoms distribution. The female condoms have been less spoken about or advertised in the municipality. Therefore, in support of the views of the participants, the female condom is scarce and to some extent not available to purchase (Shallie & Haffejee, 2021).
Health officials indicated that condoms sold at the drug stores expire because the people in the area do not like using condoms and thus do not buy them. Although condoms are manufactured under high international standards (Beksinska et al., 2017), low patronage at chemist shops increases their likelihood of getting expired (Adjei et al., 2015). They further reported that most of the drug store operators expose the condoms to direct sunlight and this can lead to holes being created in the condoms. The World Health Organization has advised that condoms should be stored in a well-ventilated area away from direct sunlight and other heat sources to reduce their exposure to high temperatures (World Health Organization, 2019). Health officials also attributed the problem of condoms getting burst during sexual intercourse to the men in the area not wearing condoms properly and also their low level of education.
The study also sought information from respondents on reasons they would not use condoms during sexual intercourse. A majority of respondents in both the rural (76.0%) and urban (74.0%) community reported that condoms get torn, female condoms are complicated to use and more importantly condoms diminish a man’s or woman’s sexual pleasure. They further explained that sexual pleasure derived when condoms are used during sexual intercourse is lower as compared to when no condoms are used. Participants expressed that:
“The feeling is definitely not the same.” (Rural resident 11)
“I feel cheated anytime I used condoms on a woman because I don’t enjoy and feel the inner flesh of the vagina.” (Urban resident 11)
It is obvious in Ghana that most of the youth are less concern about the usage of condoms and engage in unprotected sex (Manu et al., 2022). Following some findings made by some studies on diminishing pleasure with condom use, it was revealed that many men would not like to use condoms because it reduces the arousal or sensation they get from sexual intercourse (Hensel et al., 2012; Randolph et al., 2007). This views then confirms the expression of the participants.
The study also asked respondents and participants question on whether buying condom is embarrassing in LMKM. A majority of respondents in both the rural (71.4%) and urban (74.4%) community agreed that buying condom is embarrassing in the local area. They further explained that condom use is associated with deviant and immoral behaviours such as prostitution. People in possession of condoms or found using them are seen as ‘unfaithful’, ‘cheats’, ‘having something to hide’ and ‘not trustworthy’. In this regard some of the participants reported:
“To go for a condom in a drug store here, never …..this is a small community and everyone knows everyone including the seller at the drug store. I will not want people to see me as a promiscuous girl or a prostitute. When I am ready for marriage no man will want me.” (Rural resident 12)
“Most of the time as a man I find it very difficult to go to the drug store or even the health centre for condoms. If you are not married and you use condoms you are seen as a ‘womanizer’ forgetting that even if you are with one partner pregnancy can come when you are not ready. If you are married too your wife will know you bought a condom and that may spark trouble at home if your wife don’t trust you.” (Urban Resident 13)
“Getting a condom from a pharmacy or drug store operated by a lady is embarrassing but buying it from a shop where it’s a male who sells is not embarrassing. I normally don’t mind walking longer distance just to get a pharmacy operated by a man to buy a condom.” (Rural resident 13)
The findings above are consistent with a study that reported that people are shy or embarrassed to purchase condoms at the pharmacy and to some extent get interrogated by the pharmacy assistants for showing up to buy condoms (Gyan & Marhefka-Day, 2021). The persistence of this problem may cause the youth to indulge in unprotected sex and risk their lives of contracting HIV infection (Ankunda et al., 2016).
Drug store operators in the district on the other hand reported that condoms are bought by some males and females. However, most of the females who visit the drug store purchase male condoms and are not even aware that there are female condoms. As a result, they have given it various names to prevent other customers, especially children, from knowing that someone is buying condoms. This is what one drug store operator had to say:
“The buying of condoms is embarrassing so it has been given names like ‘boat’, ‘player’, ‘APC’ and ‘shingad’ etc.”
The drug store operator has brought to bear the embarrassment some people face when buying condoms. Research conducted on purchase of condom and its associated embarrassment, researchers asked people how they deal with the embarrassment of purchasing condoms, and they discovered that many responded by purchasing other products to hide the condoms, going to a cashier of the same gender, or visiting locations where condoms are distributed for free (Moore et al., 2006).
Level of educational campaigns on condom use and HIV/AIDS
Residential differentials on responses on level of educational campaigns on condoms use and HIV/AIDS was observed in the municipality. While a majority (67.8%) of rural respondents reported that the level of educational campaign on condom use as an HIV preventive measure is low in the municipality, a little over half of urban residents (54.4%) said that the level of educational campaign on condom use as HIV preventive measure is high. Municipal and local leaders further indicated that in the early 1999 when the municipality recorded HIV/AIDS prevalence of about 13%, there was widespread educational campaigns on HIV/AIDS because funding was allocated for such programmes. However, when prevalence declined to 7 percent in early 2000 funding ceased as did the HIV/AIDS awareness educational campaign (See Figure 3).
Figure 3: Signboard erected in LMKM to educate people on female condom use and HIV/AIDS prevention.
Source: Field work, 2022
One of them emphasized that the programmes were not sustained because of a lack of funds and as a result the disease prevalence among pregnant women attending antenatal clinics in the municipality has remained very high (increasing to almost 10 percent in recent times) although the national prevalence has decreased to 1.25 percent. An opinion leader explained the situation:
“When funding was available, we used to go round with some of the health officers and NGOs in the district telling people how the disease is spread and how to protect themselves by using condoms…we also taught them how to use condoms and gave out free condoms…but now no funding so I have now shifted my focus on the Dipo girls.” (Local leader)
A local leader also reported that there used to be demonstrations on how condoms are used and selling of condoms at subsidised prices when the programme was in progress. However, in recent times one has to go to the drugstore to purchase condoms at retail prices.
CONCLUSIONS
In all, urban dwellers exhibited good knowledge of and practised the ‘ABC’ model of HIV prevention in that, urban dwellers had good knowledge on abstinence, condom and used condoms as HIV preventive measures compared to rural dwellers. It can therefore be concluded that, knowledge on and practice of the ‘ABC’ model of HIV preventive practices is influenced by the residential location in LMKM. The study also found that both rural and urban dwellers misunderstood the term be faithful (B) in the ‘ABC’ model as most of them had more life time sexual partners which does not conform to the model. Factors influencing the knowledge of both urban and rural dwellers on the ‘be faithful’ concept of the ‘ABC’ model of HIV prevention model which create the misunderstanding was not explored. Scholars should consider examining the factors in that regard. It is therefore recommended that, the Municipal Health Directorate in collaboration with Ghana AIDS Commission, National Commission on Civic Education, community leaders, youth organizations and non-governmental organization should intensity the campaign on the ‘ABC’ model of HIV prevention, particularly in rural settings within the municipality.
IMPLICATIONS FOR POLICY AND PRACTICE
The study’s findings could serve as the basis for the formulation and implementation of HIV preventive campaign programmes by state agencies such as Ministry of Health, Ghana Health Service, Ghana AIDS Commission and National AIDS and STI Control Programme (NACP) and other non-governmental organizations aimed at increasing prevention knowledge and practices of rural and urban residents. This will help in preventing and controlling the spread of HIV/AIDS in the municipality.
REFERENCE
- Adjei, K. K., Laar, A. K., Narh, C. T., Abdulai, M. A., Newton, S., Owusu-Agyei, S., & Adjei, S. (2015). A comparative study on the availability of modern contraceptives in public and private health facilities in a peri-urban community in Ghana. Reproductive health, 12(1), 1-8.
- Aggarwal R, & Ranganathan P. (2019). Study designs: Part 2-Descriptive studies. Perspect Clin Res 10, 34-6.
- Ali, M. S., Tesfaye Tegegne, E., Kassa Tesemma, M., & Tesfaye Tegegne, K. (2019). Consistent condom use and associated factors among HIV-positive clients on antiretroviral therapy in North West Ethiopian Health Center, 2016 GC. AIDS research and treatment, 2019.
- Ananga, M. K., Kugbey, N., Akporlu, J. M., & Oppong Asante, K. (2017). Knowledge, acceptance and utilisation of the female condom among women of reproductive age in Ghana. Contraception and reproductive medicine, 2, 1-9.
- Ankunda, R., Atuyambe, L. M., & Kiwanuka, N. (2016). Sexual risk related behaviour among youth living with HIV in central Uganda: implications for HIV prevention. Pan African Medical Journal, 24(1).
- Apanga, P. A., Akparibo, R. & Awoonor-Williams, J.K. (2015). “Factors influencing uptake of voluntary counselling and testing services for HIV/AIDS in the Lower Manya Krobo Municipality (LMKM) in the Eastern Region of Ghana: a cross-sectional household survey.” Journal of Health, Population and Nutrition, 33 (1)
- Appiah, F., Fenteng J. O. D., Darteh A.O., Dare F, Saah J.A., Takyi M., Ayerakwah P.A., Boakye K, & Ameyaw E.K. (2022). Association between mass media exposure and endorsement of HIV-infected female teachers’ teaching: insight from 2014 Ghana Demographic and Health Survey. BMC Women’s Health. 22 (1), 121.
- Appiah-Agyekum, N. N., & Suapim, R. H. (2013). Knowledge and awareness of HIV/AIDS among high school girls in Ghana. HIV/AIDS-Research and Palliative Care, 137-144.
- Beksinska, M., Greener, R., Kleinschmidt, I., Pillay, L., Maphumulo, V., & Smit, J. (2017). A randomized noninferiority crossover-controlled trial of the functional performance and safety of new female condoms: an evaluation of the Velvet, Cupid2, and FC2. Contraception, 92(3), 261-267.
- Bell, K. (2014). HIV prevention: Making male circumcision the “right” tool for the job. Global Public Health, 10(5-6), 552–572.
- Boakye, K. E. (2009). Attitudes toward rape and victims of rape: A test of the feminist theory in Ghana. Journal of Interpersonal Violence, 24(10), 1633-1651.
- Campbell, C. (1997). Migrancy, masculine identities and AIDS: The Psychological Context of HIV Transmission on the South African Gold Mines. Social Science and Medicine. 45 (2), 273-281.
- Chae, S., & Agadjanian, V. (2022). The Transformation of Polygyny in Sub‐Saharan Africa. Population and Development Review, 48(4), 1125-1162.
- Cherie S, Workie H, Kassie T, Bitew A, & Samuel T. (2022) Pregnant Women’s Knowledge, Attitude, and Practice Towards the Prevention of Mother to Child Transmission of HIV/AIDS in Dil Chora Referral Hospital, Dire Dawa, Eastern Ethiopia: A Cross-Sectional Study. 11(14), 45-60.
- Deering, K. N., Lyons, T., Cindy, X. F., Nosyk, B., Strathdee, S. A., Montaner, J. S., & Shannon, K. (2013). Client demands for unsafe sex: the socio-economic risk environment for HIV among street and off-street sex workers. Journal of acquired immune deficiency syndromes (1999), 63(4), 522.
- Dejman M, Ardakani H. M, Malekafzali B, Moradi G, Gouya M. M, Shushtari Z. J, Alinaghi S. A, & Mohraz M. (2015). Psychological, Social, and Familial Problems of People Living with HIV/AIDS in Iran: A Qualitative Study. Int J Prev Med.6 (126).
- Elshiekh, H. F., Hoving, C., & de Vries, H. (2020). Exploring determinants of condom use among university students in Sudan. Archives of sexual behavior, 49, 1379-1391.
- Garcia, E. C., Costa, I. R., Oliveira, R. C. D., Silva, C. R. L. D., Góis, A. R. D. S., &Abrão, F. M. D. S. (2021). Social representations of adolescents about HIV/AIDS transmission in sexual relations: vulnerabilities and risks. Escola Anna Nery, 26.
- Ghana AIDS Commission (2014). National and Sub-National HIV and AIDS Estimates and Projections. 2014 Report. UNAIDS (2020). Country Fact Sheet. http://unaids.org/en/regionscountries/countries/ghana, accessed 27.10.2022
- Ghana AIDS Commission (2019). National and Sub-National HIV and AIDS Estimates and Projections. 2019 Report. UNAIDS (2020). Country Fact Sheet. http://unaids.org/en/regionscountries/countries/ghana, accessed 27.10.2022
- Ghana Statistical Service (2021). Population and Housing Census. Summary Report of Final Results.
- Gyan, S. E., & Marhefka-Day, S. (2021). Exploring Adolescents’ (Non-)Use of Modern Contraceptives in Ghana Through the Lens of the Theory of Gender and Power. Archives of Sexual Behavior, 50(6), 2411–2421.
- Halasa-Rappel, Y. A. Gaumer, G. Khatri, D. Hurley, C. L. Jordan. M. & Nandakumer, A. K. (2021). The Tale of Two Epidemics: HIV/AIDS in Ghana and Namibia. The Open AIDS Journal. 15, 63-72.
- Hensel, D.J., Stupiansky, N.W., Herbenick, D. Dodge, B., & Reece, M. (2012). Sexual pleasure during condom-protected vaginal sex among heterosexual men. J Sex Med. 9 (5),1272-6.
- Hu, L., Luo, Y., Zhong, X., Lu, R., Wang, Y., Sharma, M., & Ye, M. (2020). Condom use and related factors among rural and urban men who have sex with men in Western China: based on information-motivation-behavioral skills model. American Journal of Men’s Health, 14(1), 1557988319899799.
- Jennifer L. W. & Carrie L. K. (2010). The WHO Clinical Staging System for HIV/AIDS. AMA Journal of Ethics. 12 (3), 202-206.
- King, N (2004). Using templates in the thematic analysis of text. In Cassel, C., Symon., G (Eds.) Essential guide to qualitative methods in organizational research. London, UK: Sage.
- Koenig, L.J., Hoyer, D., Purcell, D.W., Zaza, S., & Mermin, J. (2016). Young People and HIV: A Call to Action. Am J Public Health. 106 (3), 402-5.
- Kose, S, Mandiracioglu, A, Mermut, G, Kaptan, F, & Ozbel, Y. (2012). The Social and Health Problems of People Living with HIV/AIDS in Izmir, Turkey. Eurasian J Med. 44 (1).
- Lasry, A., Sansom, S. L., Wolitski, R. J., Green, T. A., Borkowf, C. B., Patel, P., & Mermin, J. (2014). HIV sexual transmission risk among serodiscordant couples: assessing the effects of combining prevention strategies. AIDS (London, England), 28(10), 1521.
- Liu, Z., Wei, P., Huang, M., Liu, Y. B., Li, L., Gong, X., … & Li, X. (2014). Determinants of consistent condom use among college students in China: application of the information-motivation-behavior skills (IMB) model. PLoS One, 9(9), e108976.
- Lower Manya Krobo Municipal Assembly (2022). Retrieved May 18, 2022 from https://lmkma.gov.gh/
- Lower Manya Krobo Municipal Profile, (2020). Lower Manya Municipal Assembly, Odumase Krobo. Retrieved June 30, 2022 from www.lowermanyadistrict.com.
- Manu A, Ogum-Alangea D, Azilaku J. C, Anaba E. A, &Torpey K. (2022). Risky sexual behaviours and HIV testing among young people in Ghana: evidence from the 2017/2018 Multiple Indicator Cluster Survey. Reprod Health. 19(1)
- Marrazzo, J. M., & Cates, W. (2011). Interventions to prevent sexually transmitted infections, including HIV infection. Clinical infectious diseases, 53(suppl_3), S64-S78.
- Mbachu, C. O., Agu, I. C., Obayi, C., Eze, I., Ezumah, N., &Onwujekwe, O. (2021). Beliefs and misconceptions about contraception and condom use among adolescents in south-east Nigeria. Reproductive Health, 18, 1-8.
- Milic, M., Gazibara, T., Stevanovic, J., Parlic, M., Nicholson, D., Mitic, K., … &Dotlic, J. (2020). Patterns of condom use in a university student population residing in a high-risk area for HIV infection. The European Journal of Contraception & Reproductive Health Care, 25(4), 269-278.
- Mohamad Shakir, S. M., Wong, L. P., Lim Abdullah, K., & Adam, P. (2020). Online STI information seeking behaviour and condom use intentions among young Facebook users in Malaysia. Health promotion international, 35(5), 1116-1124.
- Mohammadi Gharehghani, M. A., Khosravi, B., Irandoost, S. F., Soofizad, G., &Yoosefi lebni, J. (2020). Barriers to condom use among female sex workers in Tehran, Iran: a qualitative study. International Journal of Women’s Health, 681-689.
- Moore, S. G., Dahl, D. W., Gorn, G. J., & Weinberg, C. B. (2006). Coping with condom embarrassment. Psychology, Health & Medicine, 11(1), 70–79.
- Nadarzynski, T., Burton, J., Henderson, K., Zimmerman, D., Hill, O., & Graham, C. (2019). Targeted advertisement of chlamydia screening on social media: a mixed-methods analysis. Digital health, 5, 2055207619827193.
- Nakiganda, L. J., Bell, S., Grulich, A. E., Serwadda, D., Nakubulwa, R., Poynten, I. M., & Bavinton, B. R. (2021). Understanding and managing HIV infection risk among men who have sex with men in rural Uganda: a qualitative study. BMC Public Health, 21, 1-9.
- National AIDS Control Program (NACP) & Ghana Health Service (GHS) (2011). National HIV Prevalence & AIDS Estimates Report 2010- 2015. NACP, GHS and MOH. Accra: Ghana.
- National AIDS Control Program (NACP) & Ghana Health Service (GHS) (2020). National HIV Prevalence & AIDS Estimates Report 2010-2020. NACP, GHS, and MOH. Accra: Ghana.
- NHS website. (2022). Do condoms always prevent HIV transmission? nhs.uk. Retrieved on 31st January, 2023 from https://www.nhs.uk/common-health-questions/sexual-health/do-condoms-always-prevent-hiv-transmission/
- O’Brien, J., (2017). Can faith and freedom co-exist? When faith-based health providers and women’s needs clash. Gend. Dev. 25, 37-51.
- Ocran, B., Talboys, S., & Shoaf, K. (2022). Conflicting HIV/AIDS Sex Education Policies and Mixed Messaging among Educators and Students in the Lower Manya Krobo Municipality, Ghana. Int. J. Environ. Res. Public Health.19, 15487.
- Ofori, M., Nyarne, E. A., & Eshun, I. (2022). Students’ Knowledge and Sources of Information on HIV/AIDS: Evidence from the Lower Manya Krobo Municipality of the Eastern Region of Ghana. Universal Journal of Social Sciences and Humanities. 2, 390.
- Owusu, A.Y. (2020). A gendered analysis of living with HIV/AIDS in the Eastern Region of Ghana. BMC Public Health 20, 751.
- Owusu, A.Y., & Laar, A. (2018). Managing HIV-positive sero-status in Ghana’s most HIV concentrated district: self-perceived explanations and theoretical discourse. Afr J AIDS Res. 17(1), 82-90.
- Patel, P., Borkowf, C. B., Brooks, J. T., Lasry, A., Lansky, A., & Mermin, J. (2014). Estimating per-act HIV transmission risk: a systematic review. AIDS (London, England), 28(10), 1509.
- Platt, L., Grenfell, P., Meiksin, R., Elmes, J., Sherman, S. G., Sanders, T., … & Crago, A. L. (2018). Associations between sex work laws and sex workers’ health: A systematic review and meta-analysis of quantitative and qualitative studies. PLoS medicine, 15(12), e1002680.
- Poku, A. A. (2022). Cultural Sustainability of Dipo Puberty Rite and its Associated HIV Risks in The Lower Manya Krobo Municipality in Ghana. European Journal of Social Sciences Studies. DOI: 10.46827/ejsss.v8i1.1378. 8 (1).
- Preston, D. B., D’Augelli, A. R., Cain, R. E., & Schulze, F. W. (2002). Issues in the development of HIV-preventive interventions for men who have sex with men (MSM) in rural areas. Journal of Primary Prevention, 23(2), 199-214.
- Quarm, M. E., Mthembu, J., Zuma, K., & Tarkang, E. E. (2021). Knowledge, attitudes and prevention practices regarding HIV/AIDS among barbers in Ho municipality, Ghana, SAHARA-J: Journal of Social Aspects of HIV/AIDS, 18(1), 42-51.
- Randolph, M. E., Pinkerton. S.D., Bogart, L.M., Cecil, H., & Abramson, P.R. (2007). Sexual pleasure and condom use. Arch Sex Behav. 36 (6), 844-8.
- Safeek, R.H., Hall, K.S., Lobelo, F., Del-Rio, C., Khoury A.L., Wong, T., Morey, M.C., & McKellar, M.S. (2018). Low Levels of Physical Activity Among Older Persons Living with HIV/AIDS Are Associated with Poor Physical Function. AIDS Res Hum Retroviruses. 34 (11), 929-935.
- Setia, M. S. (2016). Methodology series Module 3: Cross-sectional studies. Indian J Dermatol 61, 261-4.
- Shallie, P. D., & Haffejee, F. (2021). Systematic review and meta-analysis assessing the knowledge and use of the female condom among Nigerians. African Health Sciences, 21(3), 1362-1374.
- Shelton, J. D., Halperin, D. T., Nantulya, V., Potts, M., Gayle, H. D., & Holmes, K. K. (2004). Partner reduction is crucial for balanced “ABC” approach to HIV prevention. Bmj, 328(7444), 891-893.
- Smith, A. D., Tapsoba, P., Peshu, N., Sanders, E. J., & Jaffe, H. W. (2009). Men who have sex with men and HIV/AIDS in sub-Saharan Africa. The Lancet, 374(9687), 416-422.
- Smith, D. K., Herbst, J. H., Zhang, X., & Rose, C. E. (2015). Condom effectiveness for HIV prevention by consistency of use among men who have sex with men in the United States. JAIDS Journal of Acquired Immune Deficiency Syndromes, 68(3), 337-344.
- Stover, J., Rosen, J. E., Carvalho, M. N., Korenromp, E. L., Friedman, H. S., Cogan, M., & Deperthes, B. (2017). The case for investing in the male condom. PloS one, 12(5), e0177108.
- Sychareun, V., Vongxay, V., Houaboun, S., Thammavongsa, V., Phummavongsa, P., Chaleunvong, K., & Durham, J. (2018). Determinants of adolescent pregnancy and access to reproductive and sexual health services for married and unmarried adolescents in rural Lao PDR: a qualitative study. BMC pregnancy and childbirth, 18, 1-12.
- Teye, J. (2004). The use of Modern Contraceptives for Fertility Reduction and Control of HIV/AIDS in Ghana.A Case Study of Krobo Odumase. Master Degree Thesis NTNU Trondheim, Norway.
- Touyz, L. Z., & Touyz, S. J. (2020). Kissing, Saliva and Human Papilloma Virus: Principles, Practices, and Prophylaxis. Journal of Medical Research and Health Sciences, 3(9), 1078-1086.
- Wang, W., Alva, S., & Wang, S. (2012). HIV-related knowledge and behaviors among people living with HIV in eight high HIV prevalence countries in sub-Saharan Africa. ICF International.
- Workowski, K. A., & Bolan, G. A. (2015). Sexually transmitted diseases treatment guidelines, 2015. Morbidity and mortality weekly report: Recommendations and reports, 64(3), 1-137.
- World Health Organization. (2019). WHO/United Nations Population Fund (UNFPA) recommendations for condom storage and shipping temperatures. WHO Drug Information, 33(3), 541-561.
- Zulu, E. M., Dodoo, F. N. A., & Chika-Ezeh, A. (2002). Sexual risk-taking in the slums of Nairobi, Kenya, 1993-98. Population studies, 56(3), 311-323.
- Zuma K, Simbayi L, Zungu N, Moyo S, Marinda E, Jooste S, North A, Nadol P, Aynalem G, Igumbor E, Dietrich C, Sigida S, Chibi B, Makola L, Kondlo L, Porter S, &Ramlagan S. (2022). The HIV Epidemic in South Africa: Key Findings from 2017 National Population-Based Survey. Int J Environ Res Public Health. 19 (13).