Linguistic and Cultural Barriers Affecting Clinician-Patient Communication in Hospitals in the South West Region of Cameroon
- Mba Atche
- 2004-2017
- Dec 25, 2023
- Development Communication
Linguistic and Cultural Barriers Affecting Clinician-Patient Communication in Hospitals in the South West Region of Cameroon
Mba Atche
University of Buea
DOI: https://dx.doi.org/10.47772/IJRISS.2023.7011160
Received: 26 October 2023; Revised: 16 November 2023; Accepted: 20 November 2023; Published: 25 December 2023
ABSTRACT
This study investigated the linguistic and cultural differences that affect clinician-patient communication in the Fako Division of Cameroon. An exploratory research design was employed where simple random and purposive sampling technique to elicit data. The patients that constituted the sample were randomly selected in the hospital and administered questionnaire and interviews. Upon collection of data, Shannon-Weaver (1948) Communication Model, Ajzen (1980) Theory of Planned Behaviour and Giles’s (2016) Communication Accommodation Theory guided the analysis. The results for this study evinced that the language used by clinicians and patients in the health area of Fako varies as it involves different languages. That is, clinicians used whatever coping techniques to get their message across to the patients during clinical communication and patients are sometimes dissatisfied with the level of information they get concerning their health situations. The results also indicated that patients use different techniques to get their message across to the clinicians who sometimes find it difficult to get the intended message leaving them frustrated. Based on these results, this study recommends that: (a) the Cameroon government through the local hospital administration should train their staff in the common language mostly used by the patients in that area to foster communication between them to avoid having patients and clinician devise coping techniques to communicate with each other; and (b) the hospital should also put in place expert translators to reduce the information disparity in situations where family, friends or colleagues are used to play the role of translators.
Key words: cultural differences, linguistic differences, clinician-patient communication, coping strategies
INTRODUCTION
Communication is important in all aspects of health and welfare: from disease prevention, health promotion to quality of life (Rimal & Lapinski, 2009; Trummer et al., 2006). While good communication practices achieve better health outcomes, ineffective communication result in a good number of health problems (Rimal & Lapinski, 2009). According to Wong and Lee (2006), “Good doctor-patient communication is important and has multiple impacts on various aspects of health outcomes. Some of these impacts are: “better health outcomes, higher compliance to therapeutic regimens in patients, higher patient and clinician satisfaction, and a decrease in malpractice risk” (p. 8). Put differently, good clinician-patient communication makes a difference not only in-patient satisfaction but in-patient outcomes including resolution of chronic headaches, changes in emotional states, lower blood sugar values in diabetics, improved blood pressure readings in hypertensive but to name a few. Ha and Nancy (2010) also state that clinicians with better communication and interpersonal skills can detect problems earlier, can prevent medical crises and expensive intervention, and provide better support to their patients. According to them, this increases higher-quality outcomes and better satisfaction, lower costs of care, greater patient understanding of health issues, and better adherence to the treatment process (p.38).
Clinician-patient relationship and communication has focused on three interrelated axes: clinical care researchers, linguistic researchers and general society researchers. According to Kaba and Sooriakumaran (2007), until the 1960s, medical sources agreed that communication between clinicians and patients should be purely paternalistic. Topics of discussion between physician and patient were restricted to the cause of their illness, physicians were to converse only with patients without their friends or family members, and physicians were warned against providing the truth about their conditions. The later years however witnessed the development of strong theoretical foundations for clinician-patient relationship as there was an insight into healthcare language and better consultation: communication was patient centred. Today, patients and clinicians are beginning to find a healthier balance of power through a process of shared decision making. Studies in this dimension include empirical research on language use and interaction of patients and clinicians, their perception and experiences of their communication with one another. In this light, the discourse of analytic studies of communication have shown ways in which decisions are managed and negotiated, cultural understandings of illness, the influence of multiple languages in a consultation, and how perceptions of race, education and social class shape physician-patient relationship. Several studies have presented evidence of this (see Collins et al., 2010; Dubey & Gupta, 2015; Duffy et al., 2004; Lovell et al., 2010; Montague et al., 2013; Yohannes, 2012).
Culture affects health disparities, communication and interactions in the doctor-patient relationship, the illness experience and health care outcomes (Champaneria & Axtell, 2004). Because patients’ cultural background can influence health care, more medical schools and training programs have integrated “cultural competency” into their curricula. Clinicians who are unaware of cultural influences may not only miss important medical implications for a patient but also inadvertently exacerbate an often already tenuous therapeutic relationship. A physician’s awareness of cultural context can also affect patients’ perceptions of the quality of care they receive. Research has shown that communication and culture are important to the health care experience (see Langer, 2008; Matthew & Stephanie, 2004). Communication here goes beyond language or interpreters (Duffy, 2004): it is being cognizant of what patients bring with them – culture, context, research, policy and action (Wang, 2017). Thus, doctor-clinician communication is an important marker of health-care quality, and given the pluri-linguistic nature of Cameroon and the myriad of cultural backgrounds, including the limited number of clinicians, it is necessary to find out disparities in language and culture which could stand as a barrier to communication between clinicians and patients. There has been increased cases of people venting their anger on clinicians and hospitals. There has been a slow decline in the degree of trust and expectations between patients and clinicians. People are becoming more aware of clinicians’ effectiveness or the lack of it. Therefore, this research aims to explore the extent to which linguistic and cultural differences affect clinician-patient communication in hospitals in Fako Division of the South West Region of Cameroon.
STATE-OF-THE-ART
Copious research has been conducted to show either the effect of language in clinician-patient communication or culture and clinician-patient communication (see for example Carvalho et al., 2011; Champaneria & Axtell, 2004; Daniel et al., 2011; Getachew et al., 2014; Haerizadeh et al., 2016; Na & Rau, 2017; Shalaby et al.,2019; Stojak, et al., 2018; Zheng, 2013 to name a few). Daniel et al. (2011) assess communication skill deficiency among all categories of physicians. The study used a sample of 384 physicians is selected using a stratified random sampling method. The medical practice at Teaching Hospital shows the existence of palpable communication skill deficiency among all categories of physicians. Carvalho et al. (2011) examine the effects of communication skills program on professional practitioners’ performance and self-confidence in clinical interviewing. The data collected for this study involve 25 health professionals who took 3 months of basic communication skills followed by 3 months of advanced communication skills and the results for this study indicate that the program improved communication skills, even though significantly only when assessed by external observers. Studies like Getachew et al. (2014) have also presented similar findings.
Contrary to the above, Roter and Hall (1995) demonstrate that, besides language, there are other factors which help strengthen the doctor-patient relationship. These factors include: laughter, jokes, making personal remarks, giving the patient compliments, friendliness, honesty, a desire to help, devotion, a non-judge mental attitude and a social orientation. Silverman and Kinnersley (2010) also contend that verbal communication in medical consultations is well recognised as being important to the delivery of medical care and is usually easy to interpret and analyse. One should not be surprised, therefore, that non-verbal communication plays a significant role throughout the medical interview and is an important variable in doctor-patient interactions. en concerns and emotions, and helps to reinforce or contradict our verbal comments.
Zheng (2013a, 2013b) has also shown that cultural differences between U.S. physicians and international patients can cause misunderstandings or discomfort during their communication. Brown (2006) also examines the impact of ethnic identity on how physicians and patients communicate in the medical interview based on the tenets of the Communication Theory of Identity. The study an apparent connection between ethnic identity salience and intensity and effective intercultural communication and satisfaction for physicians and patients may not have strongly appeared in the above study. Löffler-Stastka et al. (2016) further assess gender-specific differences in the attitudes towards doctor-patient communication among medical students and physicians. Their findings however are consistent with the fact that study a gender-dependent communication style is influenced by stereotypes.
METHODS
This study is exploratory, and relied mostly on the qualitative approach for data collection. This was because the focus of data collection was to obtain rich descriptions of individual doctor-patient experiences to enable us explain the phenomena under study. The qualitative approach was adopted because we sought to examine the experiences, perspectives and perceptions of clinicians and patients to enable us answer the following research question: To what extent do linguistic and cultural differences affect clinician-patient communication in hospitals in Fako Division of the South West Region of Cameroon? This enabled us to collect data from patients and clinicians about their background, their language and other cultural diversities to their opinions and experiences or previous experiences during medical encounters, observing their attitudes and tabulating their answers. Our sample thus comprised 170 participants. 50 respondents were in-ward patients and 60 were out-ward-patients. The remaining 60 questionnaire was done on people who were neither sick nor in a hospital environment at the moment but who had got sick and seen a clinician before. The ultimate goal of this design is to learn about a larger Cameroonian population by surveying a sample of that population in Fako Division.
This research combined qualitative and quantitative research methods in order to investigate the research questions and enhance trustworthiness through triangulation. The study further used simple random sampling and purposive sampling techniques. We randomly picked patients at the hospital and administered (those who were willing and administered the questionnaire. Again, a simple random sampling was done where we were allowed to approach the closest individuals to serve as informants in our investigation. The criterion purposeful sampling was used in the identification and selection of potential participants. These individuals were selected based on the assumption that they possess knowledge and experience with the practices or phenomenon of interest and for that reason, could be able to provide information that is both detailed and generalizable (Palinkas et al., 2015). These key resource persons were to ascertain the assertion that some cultural norms, belief systems and practices may interfere with their healthcare practices. This was the case of the Muslim religion, churches like the Apostolic Faith church, Jehovah witness, Catholic Church, Presbyterian Church and the True church of God of prophecy. Interviews were done with three information-rich cases (Palinkas et al., 2015) of each of the institutions. Madey (1978) suggests that using a mixed method design can strengthen each method by using intrinsic qualities of each other. For data collection, we made use of questionnaire and the focus group discussions as our major instruments. However, they were backed and followed by the administration of an interview being a qualitative instrument (as data for this study is part of an ongoing PhD thesis). At the level of analysis, data collected were given numerical values and figures were corroborated with other responses which were grouped in themes for proper interpretation. After analysis, information got through the use of these instruments was integrated at the level of interpretation. Upon presentation of the data, our interpretation was guided by Giles’ Communication Accommodation Theory, Shannon-Weaver’s Communication Model, and the Theory of Planned Behaviour.
RESULTS
Table 1. Patients’ language use with clinicians
| language used in communicate | Total | ||||
| Other | Pidgin | French | English | ||
| FSLC | 3 | 28 | 8 | 4 | 43 |
| O/L | 0 | 6 | 3 | 21 | 30 |
| A/L | 0 | 1 | 3 | 18 | 22 |
| BSc/BA | 0 | 2 | 3 | 14 | 19 |
| MSc+/MA+ | 0 | 2 | 2 | 8 | 12 |
| Others | 2 | 18 | 7 | 5 | 32 |
| Total | 5 | 57 | 26 | 70 | 158 |
We noticed that of the 43 patients with First School Leaving Certificate (FSLC), 28 of them used CPE in communicating with the clinician while 8 of them made use of French, 4 made use of English and 3 used other languages. Patients with Ordinary Level of Education (O/L) mostly used English. That is, out of the 30 patients with this level of education, 21 used English language, 3 used French language and 6 used CPE in communicating with the clinicians. Talking about patients with Advanced Level (A/L), 22, 18 used more of English language, 3 used French language and just one person indicated the use of CPE. Those with Bachelors and Master’s degrees used English primarily in communicating with the clinician.
It was clear that the most popular language used by the sampled patients in communication with clinicians within Fako was English language though comparatively, CPE tended to dominate when the patient involved had not attained at least a secondary school level in education.
Table 2. Clinician-patient language use in communication
| Patient Language use | Total | |||||
| Other | Pidgin | French | English | |||
| Physician
Language use |
Other | 1 | 2 | 1 | 0 | 4 |
| Pidgin | 0 | 22 | 1 | 1 | 24 | |
| French | 0 | 2 | 17 | 3 | 22 | |
| English | 4 | 31 | 7 | 66 | 108 | |
| Total | 5 | 57 | 26 | 70 | 158 | |
We noticed that while there were 108 patients who claimed that their clinicians communicated with them in English language, there were only 70 patients who indicated that they used English language in their communication with the clinician. Thus, 66 patients claimed that they used English language while their clinician used the same English language in response. 31 patients used CPE while their clinician used English language in return, 7 patients spoke in French with their clinicians who then used English in response. Again, there were 4 patients who used other languages but their clinicians responded in English Language.
Another important point here was that of the 57 patients who spoke to their clinician in CPE just 22 of them got a response in the same language. For the French speaking patients, out of the 26, 17 got their responses in French, 7 in English and 2 in CPE.
Table 3. Patient understanding of clinicians
| Response | Frequency | Per cent | Cumulative Per cent |
| No
moderately Yes Total |
43 | 27.2 | 27.2 |
| 65 | 41.1 | 68.4 | |
| 50 | 31.6 | 100.0 | |
| 158 | 100.0 |
The results (in table 3 above) showed that there were 43 (27.2%) of the patients who indicated that they did not understand their clinician and 65 (41.1%) responded that they moderately understood their clinician. However, 50 (31.6%) of the respondents indicated that they understood their clinicians so well. Based on the responses provided in the table, a cumulative 68.4% of the respondents did not understand or moderately understood their clinicians. However, in our focus group discussion, some clinicians suggested that whenever they realized that the patient did not understand them, they rephrased the question. A female doctor sighted a case when she asked a woman; “madame, weti bring you for hospital?” and the lady replied; “na okada,” when she actually meant to ask the health problem that brought the lady to the hospital. “In such cases, the clinician should be smart and quickly rephrase the question in order to get the right answer”, added another doctor.
Table 4. Patients’ perception of clinicians’ attention during consultation
| Did the clinician listen to you carefully during the consultation? | Total | |||
| No | Yes | |||
| What is your level of Education? | FSLC | 37 | 6 | 43 |
| O/L | 19 | 11 | 30 | |
| A/L | 4 | 18 | 22 | |
| Bsc | 8 | 11 | 19 | |
| Msc+ | 0 | 12 | 12 | |
| Others | 21 | 11 | 32 | |
| Total | 89 | 69 | 158 | |
The table shows that out of the 158 respondents sampled, 89 felt that clinicians did not carefully listen to them during consultation. The table equally shows that for the most part, those who held this belief were of a lower level of education. All the Master Degree holders, a majority of the Bachelor and Advanced level holders indicated that clinicians carefully listened to them during consultation.
Table 5. Patients’ Satisfaction with clinicians’ understanding of their problems
| Would you like to visit the same physician in future for your health? | Total | |||
| No | Yes | |||
| Give your reason(s) | Good Diagnosis | 0 | 4 | 4 |
| Soft Spoken | 0 | 6 | 6 | |
| Expertise | 0 | 6 | 6 | |
| Calm and understanding | 0 | 8 | 8 | |
| Too inquisitive | 19 | 0 | 19 | |
| Show concern | 0 | 5 | 5 | |
| Secretive | 0 | 5 | 5 | |
| Relative | 0 | 3 | 3 | |
| No explanation | 6 | 0 | 6 | |
| Communication problem | 24 | 0 | 24 | |
| Problem of Understanding | 13 | 0 | 13 | |
| A physician is a physician | 15 | 0 | 15 | |
| Impatient | 20 | 0 | 20 | |
| Failure to explain my worries | 24 | 0 | 24 | |
| Total | 124 | 34 | 158 | |
The table shows that 34 (21.5%) of the patients were not satisfied with the clinicians’ understanding of their problems while 55 (34.8%) expressed moderate satisfaction over clinicians’ understanding of their problems. Again, 69 (43.7%) of the patients indicated that they were satisfied with the clinicians’ understanding of their problems.
Table 5. Visit to the same physician or not and reason
| Would you like to visit the same physician in future for your health? | Total | |||
| No | Yes | |||
| Give your reason(s) | Good Diagnosis | 0 | 4 | 4 |
| Soft Spoken | 0 | 6 | 6 | |
| Expertise | 0 | 6 | 6 | |
| Calm and understanding | 0 | 8 | 8 | |
| Too inquisitive | 19 | 0 | 19 | |
| Show concern | 0 | 5 | 5 | |
| Secretive | 0 | 5 | 5 | |
| Relative | 0 | 3 | 3 | |
| No explanation | 6 | 0 | 6 | |
| Communication problem | 24 | 0 | 24 | |
| Problem of Understanding | 13 | 0 | 13 | |
| A physician is a physician | 15 | 0 | 15 | |
| Impatient | 20 | 0 | 20 | |
| Failure to explain my worries | 24 | 0 | 24 | |
| Total | 124 | 34 | 158 | |
Table 6. Patients’ reasons for Preferring an Herbalist
| Give your reason(s) | Are there any illnesses which you would prefer to consult with an herbalist and not a clinician? |
| Hepatitis B | 7 |
| Typhoid | 10 |
| Side pain | 12 |
| Better understanding | 5 |
| Some illnesses are better understood by herbalist | 12 |
| Quick and faster results | 13 |
| Traditional belief and custom | 15 |
| Herbs are better than drugs | 11 |
| We speak a common language | 11 |
| Illnesses that require spiritual consultation | 10 |
| It is easier and less expensive | 11 |
| Total | 117 |
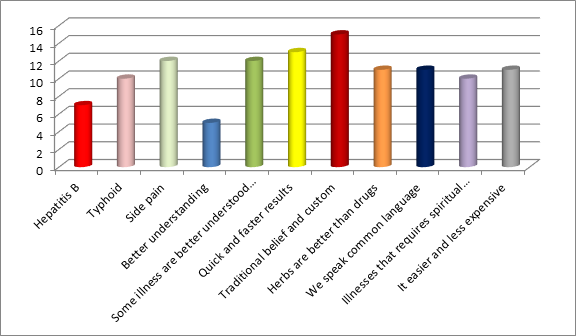
While over 27 of the respondents visited herbalists for specific illnesses, 5 of the respondents visited herbalist for better understanding of their sickness. The bar chart below shows the various reasons and we can see that the most popular reason is triggered by traditional beliefs and customs.
Figure 1. Visit to the same physician or not and reason
“Better understanding” is the least popular reason that accounted for their preference for herbalists. While besides tradition, most of them believed side pain was better treated by a herbalist and some illnesses needed spiritual consultations. Others equally believed that some illnesses were better understood by an herbalist because they spoke a common language with these herbalists. Another popular reason was the idea that herbalists provided quick and faster results and were easier and less expensive.
During the focus group discussions with some Muslims, we realized that Muslims believed more in the prevention of diseases. For this reason, they took a lot of herbs. However, the participants pointed out that there were no rules that discouraged people from going to the hospital to seek medical help.
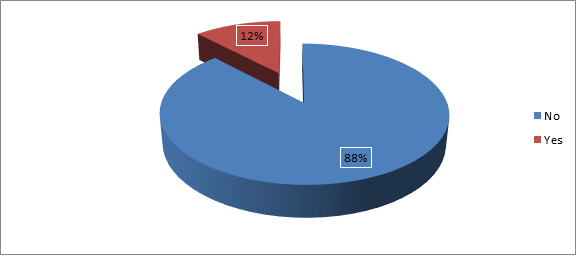
Figure 2. Illnesses which beliefs prevent you from seeking medical attention
From the figure above, we noticed that 88% of the respondents hold that there were no illnesses which (superstitious) beliefs stopped them from obtaining medical attention. However, 12% of the respondents did not receive medical attention for certain illnesses due to superstitious beliefs. Thus, it was important to point out that while most of the patients consulted with herbalists for several reasons, one of which was based on their tradition and custom as advanced in Table 4.17, only few failed to seek medical attention because of their superstitious beliefs.
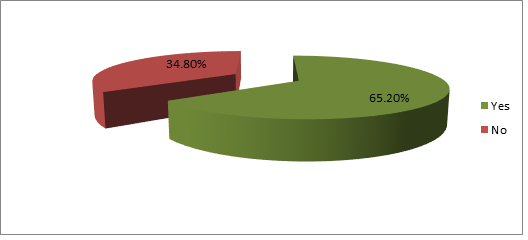
Figure 3. Medical practices forbidden by your religion or culture
From the figure above, 65.20% of patients specified that their religion or culture forbade certain medical practices, while 34.80% suggested that their religion or culture did not forbid any medical practices.
Table 6. Communication between persons using the same language is more effective
| Frequency | Per cent | |
| Strongly Disagree | 3 | 1.9 |
| Disagree | 17 | 10.8 |
| Agree | 54 | 34.2 |
| Strongly Agree | 84 | 53.2 |
| Total | 158 | 100.0 |
Most of the patients (53.2%) strongly agreed with the statement that using the same language in communication lead to effective communication, whereas 34.2 agreed with this statement giving a total of 87.4% in agreement to this fact. Only 1.9% strongly disagreed and 10.8% disagreed which implied only 12.6% of the patients were in disagreement to this statement. This information is presented on a bar chart as follows.
Table 7. Medical jargon and effective communication
| Frequency | Per cent | Cumulative Per cent | |
| Strongly Disagree | 51 | 32.3 | 32.3 |
| Disagree | 82 | 51.9 | 84.2 |
| Agree | 16 | 10.1 | 94.3 |
| Strongly Agree | 9 | 5.7 | 100.0 |
| Total | 158 | 100.0 |
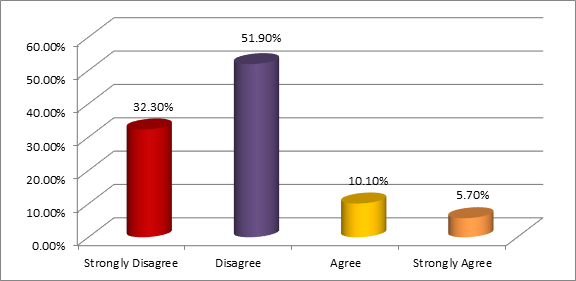
The table shows that 51 (32.3%) of the patients strongly disagreed with the fact that the use of medical jargon by clinicians lead to effective communication with their patients. 82 (51.9%) disagreed with this opinion giving a total of 84.2% of the patients in disagreement to this statement. Only 15.2% of the respondents agreed with this statement. Figure 4 below depicts this information.
Figure 4. Whether medical jargon deters effective communication with their patients
Thus, from these responses we see that most patients did not understand medical personnel who made use of medical jargons in communicating with them. This implies that physicians should try to keep their conversation very simple and free from medical terms that cannot easily be understood by most patients as this deters understanding. If they must use these terms, they should endeavour to break them down to the patients’ understanding.
Table 8. Clinicians who make use of different languages during consultation do communicate well
| Frequency | Per cent | Cumulative Per cent | |
| Strongly Disagree | 15 | 9.5 | 9.5 |
| Disagree | 17 | 10.8 | 20.3 |
| Agree | 50 | 31.6 | 51.9 |
| Strongly Agree | 76 | 48.1 | 100.0 |
| Total | 158 | 100.0 |
From the table, we realise that in most cases, the patients agreed that clinicians who used different languages in consultation tended to communicate more effectively. 76 (48.1%) of the respondents strongly agreed with this statement, while 50 (31.6%) agreed, making a total of 126 (79.7%) of the patients who held that code-switching by clinicians lead to effective communication with patients. 15 (9.5%) of the respondents strongly disagreed while 17 disagreed giving us 32 (20.3%) of the patients who did not believe that code-switching enhanced communication. The diagram below better illustrates the recorded findings.
Table 9. Communication tends to be effective between patients and clinicians of the same sex
| Frequency | Per cent | Cumulative Per cent | |
| Strongly Disagree | 4 | 2.5 | 2.5 |
| Disagree | 17 | 10.8 | 13.3 |
| Agree | 53 | 33.5 | 46.8 |
| Strongly Agree | 84 | 53.2 | 100.0 |
| Total | 158 | 100.0 |
This table shows that 17 (13.3%) of the respondents disagreed with this assessment and 4 (2.5%) strongly disagreed. Based on the responses, we noticed that 53 (33.5%) of the respondents agreed that communication tended to be more effective between patients and clinicians of the same gender, while 84 (53.2%) strongly agreed to this statement. Following our focus group discussion with clinicians, they attested to the fact that most patients tended to feel more comfortable and freer to discuss health problems with a clinician of the same gender than the opposite one.
Table 10. Patients’ illness and communication
| Frequency | Per cent | Cumulative Per cent | |
| Strongly Disagree | 3 | 1.9 | 1.9 |
| Disagree | 8 | 5.1 | 7.0 |
| Agree | 63 | 39.9 | 46.8 |
| Strongly Agree | 84 | 53.2 | 100.0 |
| Total | 158 | 100.0 |
The table shows that most of the patients agreed with the fact that patients’ communication with clinicians was affected by the type of sickness involved. This means that some patients found it difficult to reveal their situation to their clinicians. 63 (39.8%) respondents agreed with this statement while 84 (53.2%) of the respondents strongly agreed. However, 11 (7%) of the respondents disagreed with this assessment. From our focus group discussion, doctors listed some problems which patients found difficult to open up about to the clinician. They were diseases concerning sexuality (erectile dysfunction, urinary tract problems, and STDs, and infertility (especially damages caused by crude abortions and false pregnancies). To quote the words of one doctor, “while some dribble the doctor avoiding the truth, others get shy and do not want to open up.” Here, the clinician therefore has to be patient and tactful in handling.
Table 11. Patients and clinicians from the same cultural background
| Frequency | Per cent | Cumulative Per cent | |
| Strongly Disagree | 7 | 4.4 | 4.4 |
| Disagree | 15 | 9.5 | 13.9 |
| Agree | 54 | 34.2 | 48.1 |
| Strongly Agree | 82 | 51.9 | 100.0 |
| Total | 158 | 100.0 |
22(13.9%) of the respondents disagreed with this statement which implied that their communication with a clinician was not affected despite of cultural differences. Many patients agreed with this statement thereby holding that, their communication with clinicians from the same cultural background was more effective. 54 (34.2%) agreed with this while 82 (51.9%) of the patients strongly agreed. Furthermore, following a discussion with clinicians, they explained that they did their best to identify the tribes of old and timid looking patients by looking at their names. Then they would try and say a word or two in their native language (if they could) to make them feel relaxed and open up for discussion. This patient then felt like he/she was “sitting in front of his son or daughter,” thus their trust was gained. A good rapport was easily established and this restored the health of the patient. The diagram below shows the percentages of the various responses.
DISCUSSION OF FINDINGS
The study found that both patients and clinicians in Fako made use of a variety of languages in their communication with each other. Some of these languages are English language, French language, Pidgin-English and others such as native languages in situations where both patients and clinicians were from the same village or tribe and also when the patient (who could neither speak English, CPE nor French) came with someone to help in interpretation. However, the most popular language used was English language followed by CPE for most patients. We noticed that there was a disparity in the language used between patients and clinicians. In some cases, patients used CPE while clinicians responded in another language (English or French). This resulted in some patient/patients claiming not to have understood each other well during communication. In light of such difficulties, 62% of the patients felt that clinicians were unable to diagnose their problem(s) rightly though some clinicians were of the contrary opinion as they mentioned in the focus group discussions that they usually called for an interpreter whom, though not medically trained, was always ready to help in such circumstances. This is in line with Bel as en (2017) who explores the extent to which improving doctor–patient communication can address and alleviate healthcare delivery inefficiencies. The author surveys causes and costs of miscommunication including perceptual gaps between how physicians believe they perform their communicative duties versus how patients feel and highlight thresholds such as the Hospital Consumer Assessment of Healthcare Providers and Systems used by hospitals to identify health outcomes and improve doctor–patient communication.
The clinicians further mentioned that they were ready to code switched whenever they could, to use a language suitable to the patient. Thus, language used by clinicians and patients was found to be significant in the communication process between clinicians and patients. This finding was remarkably similar with Chia (2001) who found that language problems were found at the levels of description and understanding of patients’ problems. He (Chia, 2001) found out that about 10% of patients could neither express themselves in any of the country’s official languages. Thus, putting the results of Belasen (2017) who found that doctor–patient communication correlates with better and more accurate care as well as with more satisfied patients and those of Chia (2001) side-by-side who utilize an assessment framework, doctor–patient communication assessment, we note that there is evidence that doctor–patient communication strongly predicts clinical outcomes as well as patients’ overall ratings (the choice to visit the same hospital subsequently).
While this may be the case, it is still true that giving explanations to the patient about the choice of treatment, the positive and negative effects of treatment or care strategy was a point of concern to patients. The fact that 59.34% (54) patients indicated that their clinicians failed to give them any explanation about the positive and negative effects of their treatment or care strategy, and 40.66% (37) patients who also claimed their clinician moderately explained the reasons for the choice of their care strategy suggest a problem at the level of language. This finding takes us to Ciubotaraşu-Pricop the (2013) examine doctor-patient communication as the basis of health communication matrix, regardless the level at which it takes place – national, international or global. Ciubotaraşu-Pricop the (2013) employs a common communication development paradigm to tests this Metrix. Firstly, it attempts an approach to doctor-patient communication starting from the communicational paradigm, supporting the possibility of convergence of communication theories based on interrogative strategies essential to any kind of communication. The results, which we find relevant here show that doctor-patient communication strategies based on interrogative questions as a way to use communication flow takes into account a broader perspective on the structure of the question and integrates not only what is essential in the question itself, but also the elements that complete the answer / answers and what becomes specific to this type of communication, namely the listening. This as Ciubotaraşu-Pricop the (2013) explains is because interrogative communicative action type creates a reductionist effect: the questions, the answers agglutinate forming problems.
The study found out that the use of medical jargon was not welcomed as 84.2% patients disagreed that the use of medical jargon during consultations let to effective consultation. This made them to leave the room unsatisfied. This ties with Chia (2001), who opines that instances of medical jargon only demonstrate possibilities of communication breakdown and consequently wrong diagnosis leading to wrong prescription. However, some of the patients/clinicians held that communication with clinicians/patients who could switch from one language to another during clinical communication tended to be effective. Apart from Chia (2001), even more recently, our findings corroborate with those of Yohannes (2012) who investigates the sociolinguistic and pragmatic aspects of doctor-patient communication, focusing on terminology, register, turn taking, solidarity and status, language and group membership and code switching in language, and presents the following conclusions:
- The communication in the health centre is doctor-centred communication, which makes the patient a passive participant of the communication.
- In most interactions, doctors or medical professionals have a unique position of respect and power. Those are shown in decision making for the patients by their own, by asking series of close-ended questions that are focused on the doctors’ interests rather than questions that let patients to speak up about their problem or feeling.
- Most of the medical professionals at health centres show obvious communication skill deficiency in all categories. Because they use the traditional concept (Doctor-centred communication approach) that are restricted to physical illness and its intervention and treatment (pp. 131-132).
Again, following the focus group discussions with clinicians, some of them made it clear that they would readily switch to the language and level of the patient to ensure understanding. To emphasize the importance of communication in physician-patient relationship, Travalan et al. (2005) posit that since communication is often neglected in medical schools especially after 5 years of studies, there is under or poor development in this area. They found out that a language course which dealt with medical jargons was relevant as part of the curriculum.
IMPLICATIONS OF THE FINDINGS
The findings obtained in in study undoubtedly have implications for clinician-patient communication. Given that religious, traditional, family and other beliefs did affect the clinician-patient communication, even though clinicians expressed a need for patients to drop aspects of their tradition, family and religious beliefs which hindered medical procedures, there is a concern. This is more so because superstitious beliefs had resulted in most patients failing to reveal aspects of their health conditions or refusing to adopt certain health procedures or prescribed treatment. This implies that increasing the doctors’ awareness of the communicative differences and by empowering patients to express concerns and preferences, a more effective clinician-patient communication could be established. The study suggests that at both national and organization levels, policies should be in place to integrate cultural competence into health care services. Based on cultural differences also, our findings suggest that physicians have to encourage patients to discuss their concerns and to ask questions, and they should listen actively. Communication skills and attitudes training can be an important tool to improve these defaults.
REFERENCES
- Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50, 179–211.
- Belasen, A. (2017). Doctor-patient communication: A review and a rationale for using an assessment framework. Journal of Health Organization and Management, 7, 1-17. doi.org/10.1108/JHOM-10-2017-0262
- Carvalho, I., Pais, V., Almeida, S., Rebeiro-Silva, M., Teles, A., Castro-Vale, I., & Mota-Cardoso, R. (2011). Learning clinical communication skills: Outcomes of a program for professional practitioners. Patient Education and Counselling, 84-89.
- Champaneria, M. C., & Axtell, S. (2004). Cultural competence training in US medical schools. Journal of the American Medical Association, 291(17), 22-34.
- Chia, E. (2001). Doctor-patient communication in a multilingual setting. African Journal of Applied Linguistics, 2, 91-105.
- Ciubotaraşu-Pricop the, L. (2013). Interrogative strategies of doctor – patient communication. Outlook on Communication, 3(4), 310-316.
- Collins, S., Peters, S., & Watt, I. (2010). Medical communication. Routledge.
- Dubey, A., & Gupta, S. (2015). Characteristics of communication of doctors during consultation. Asian Journal of Social Sciences, Arts and Humanities, 3(2), 35-43.
- Duffy, F. D., Gordon, G. H., & Whelan, G. (2004). Assessing competence in communication and interpersonal skills: The Kalamazoo II report. Academic Medical Journal, 79(6), 495–507.
- Getachew, G., Birhan, T., Wudneh, H., Gerezgiher, B., & Haftu, B. (2014). Nurse-physician work relationships and associated factors in public hospitals in Tigray region, northern Ethiopia: A cross sectional study. Greener Journal of Biomedical and Health Sciences, 1(1), 1-13
- Giles, H. (2016). Communication accommodation theory. The International Encyclopedia of
Communication Theory and Philosophy.
https://doi.org/10.1002/9781118766804.wbiect056 - Ha, J. F., & Nancy, L. (2010). Doctor-patient communication: A review. The Ochsner Journal, Academic Division of Ochsner Clinic Foundation, 10, 38–43.
- Haerizadeh, M., Moise, N., Chang, B., Edmondson, D., & Kronish, I. (2016). Depression and doctor-patient communication in the Emergency Department. Gen Hosp Psychiatry, 42, 49–53. doi:10.1016/j.genhosppsych.2016.06.004
- Kaba, R., & Sooriakumaran, P. (2007). The evolution of the doctor-patient relationship. International Journal of Surgery, 5(1), 57-65.
- Langer, N. (2008). Integrating compliance, communication, and culture: Delivering health care to an aging population. Educational Gerontology, 34(5), 385-396. doi: 10.1080/03601270701838381
- Lovell, B.-L., Lee, R. T., Brotheridge, C.-M. (2010). Physician communication: Barriers to achieving shared understanding and shared decision making with patients. Journal of Participatory Medicine, 2, e12-e21.
- Löffler-Stastka, H., Seitz, T., Billeth, S., Pastner, B., Preusche, I., & Seidman, C. (2016). Significance of gender in the attitude towards doctor-patient communication in medical students and physicians. Springer. doi: 10.1007/s00508-016-1054-1
- Madey, D. L. (1982). Some benefits of integrating qualitative and quantitative methods in program evaluation, with illustrations. Educational Evaluation and Policy Analysis, 4(2), 223–236. https://doi.org/10.3102/01623737004002223
- Matthew, W. K., & Stephanie, M. (2004). The role of culture in health communication. Annual Review of Public Health, 25(1), 439-455. doi: 10.1146/annurev.publhealth.25.101802.123000
- Montague, E., Chen, P., Xu, J., Chewning, B., & Barrett, B. (2013). Nonverbal interpersonal interactions in clinical encounters and patient perceptions of empathy. Journal of Participatory Medicine, 5, e33-e41.
- Na, S. & Pei-Luen, P. R. (2017). Barriers to improve physician–patient communication in a primary care setting: Perspectives of Chinese physicians. Health Psychology and Behavioral Medicine, 5(1), 166-176. doi: 10.1080/21642850.2017.1286498.
- Palinkas, L. A., Horwitz, S. M., Green, C. A., Wisdom, J. P., Duan, N., & Hoagwood, K. (2015). Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Administration and Policy in Mental Health, 42(5), 533–544. https://doi.org/10.1007/s10488-013-0528
- Rimal, R. N., & Lapinski, M. K. (2009). Why health communication is important in public health. Bull World Health Organ, 87(4), 247-247. doi: 10.2471/blt.08.056713
- Shalaby, S., Saied, S. & Zayed, H. (2019). Physician-patient communication: Perception and practice among doctors working in Tanta University Outpatient Clinics. Egyptian Journal of Occupational Medicine, 43. doi:10.21608/ejom.2019.47867
- Shannon, C. E., & Weaver, W. (1949). The mathematical theory of communication. University of
Illinois Press. - Soliz, J., & Giles, H. (2012). Communication accommodation theory: A contextual and meta-analytical review. Penguin.
- Trummer, U. F., Mueller, U. O., Nowak, P., Stidl, T., & Pelikan, J. M. (2006). Does physician-patient communication that aims at empowering patients improve clinical outcome? A case study. Patient Education and Counseling, 61(2), 299-306.
- Wang, C. (2017), Interpreters = cultural mediators? Translato Logica: A Journal of Translation, Language and Literature, 7(2), 93-114
- Yohannes, A. (2012). Medical professional-patient communication in outpatient department of Kotebe health centre: A sociolinguistic and pragmatic study (Unpublished Thesis). Addis Ababa University, Addis Ababa.