Management of Psychological Distress among Cancer Patients: A Study at Kilimanjaro Christian Medical Center (KCMC) in Moshi Municipality, Kilimanjaro Tanzania.
- Mr. Godfrey Livingstone. Mbowe
- Dr. Simion Ambakisye
- Dr. Dorothy. Lubawa
- 263-281
- Nov 30, 2023
- Psychology
Management of Psychological Distress among Cancer Patients: A Study at Kilimanjaro Christian Medical Center (KCMC) in Moshi Municipality, Kilimanjaro Tanzania.
Mr. Godfrey Livingstone. Mbowe, Dr. Simion Ambakisye, Dr. Dorothy. Lubawa
Department of Education, Mwenge Catholic University
DOI: https://dx.doi.org/10.47772/IJRISS.2023.7011021
Received: 06 September 2023; Revised: 17 September 2023; Accepted: 22 September 2023; Published: 30 November 2023
ABSTRACT
Introduction: The major aim of this study was the management of Psychological Distress among Cancer Patientsat Kilimanjaro Christian Medical Center in Moshi Municipality, Kilimanjaro Tanzania. The specific objectives were to determine the management of psychological distress among cancer patients at Kilimanjaro Christian Medical Center, and to explore the relationship between demographic characteristics of cancer patients.
Methodology: The study used a sample of 175 respondents (cancer patients) and eight participants. The systematic sampling techniques used to get 175 respondents and purposively sampling techniques used to get eight participants. The study was cross-sectional design, which employed both approaches; a quantitative and qualitative approaches. The data gathered for the study were analyzed using quantitative data analyzing software SPSS version 20 and were visually presented using descriptive statistics such as frequency distribution of tables, and figures and qualitative data done through thematic analysis.
Result: The findings of the study showed that the majority of the respondents 142 (81.1%) were not received psychological distress management 33 (25.3%) respondents they received psychological distress management but 31 (19.3%) received encouragement from medical staff; either a nurse or doctor, not official psychological management to cancer patients with psychological distress. Only 2 (6%) received an official psychological management, a Cognitive Behavioral Therapy (CBT).
Conclusion and recommendation: The study recommends that it is important to involve psychological counsellors in the multidisciplinary team for treating cancer patients to address psychological distresses or issues them experiencing. Also, more research on psychological distress management should be done so to improve psychological well-being to cancer patients.
Keywords: Cancer, Management, Psychological Distress.
INTRODUCTION
Cancer is a leading causes of death worldwide for nearly 10 million death in 2020 year and the type of cancer which lead for death were lung cancer (1.80 million death), colon and rectum cancer (916000 death), liver cancer (830,000 death), stomach (769000 death) and breast cancer (685000 death (WHO, 2022).The common cases reported by WHO, (2022) were breast cancer 2.26 million, lung cancer 2.21 million, colon and rectum cancer 1.9 million, prostate cancer 1.41 million, skin cancer (non-melanoma) 1.20 million and stomach cancer 1.09 million. In 2023 year 1,958,310 new cancer cases and 609,820 cancer deaths are projected to occur in the United States of America. Siege et al. (2023).
In African continent, it estimated that more than 1.1 million people will be dying from cancer annually in 2030 (WHO, 2022). Estimated cancer incidence has doubled in sub-Saharan Africa over the past 30 years, leading to more than 520 000 deaths in 2020. Factors driving the increases include infection; aging populations; behavioral changes such as diet, alcohol use, and smoking; environmental exposures; and genetic (Larkin, 2022).
According to WHO report in 2022, in Tanzania there were more than 26000 death from cancer and over 90 percent of cancer patients reports in hospital when the disease is at advanced stage (WHO, 2022).
Oncology or cancer patients have various psychological problems such as emotional liability, changes in future perspectives, feelings of loneliness, abandonment, stigmatization and interpersonal problems (Bras., 2008) and the impact of psychological distress has been increasingly associated with poor adherence to therapy, quality of life and cancer prognosis (Srikanthan et al., 2019). The management of patients with cancer should include their psychological well-being such as (Davies & D’Arcy, 2013). The psychological management of patient with cancer differ depending on the specific disorder, whether that be psychological distress an adjustment disorder, an anxiety disorder, and depressed disorder (Holland & Alici, 2013). Psychological intervention approach in treated oncology patients comprises work with patients, from the diagnosis till the end of treatment by working with the medical team. Psychoanalytic knowledge greatly contributed to understanding of unique personality in the structured of the patient, specific models of stress response, unique defense mechanisms, and memory as a result of unique experiences, fantasy, desire, dreams, thoughts and feelings (Neuburger, 2000). Psychotherapeutic approach worked with cancer patients on defining personality structure, dealing with current situations, and identifying life events and crisis which stress patient. The aim of psychotherapeutic interventions during treatment of oncology patients was reducing and removing difficulties and bringing psychic stability (Gregurek, 2006).
The supportive psychotherapy was the cornerstone for emotional support to patients with cancer, additional psycho-therapeutic and psychiatric interaction should be provided depending on the needs of the patient (Barlow, Durand & Hofmann, 2018). The selections of intervention were done in relation to several variables include clinical psychological condition; the type and phase of illness and situation as well as availability of psycho-oncology services with trained professional (Grassi, Johansen, Annunziata et al., 2013). The psychotherapeutic intervention in oncology benefits in reduced the severity of psychological or psychiatric symptoms as well as somatic symptoms and improved quality of life well-being (Henningsen, 2018). The intervention included the supportive-expressive group psychotherapy (Classen, Kraemar, Blasey, et al., 2008), cognitive behavioral therapy (Johnson, Hopwood, Cesario et al., 2017) cognitive–existential therapy (Kissene, Bloch, Smith et al, 2003), the meaning-central psychotherapy and mindfulness stress reduction program (Breitbart et al., 2015).
The major concern of this study, therefore, is tomanage psychological distress in cancer patients who identify through clinic of cancer patients at Kilimanjaro Christian Medical Center (KCMC). KCMC is one of zonal hospital in the northern part of Tanzania which conduct clinic for the cancer patients both adult and children. The management of psychological problems facing cancer patients will help to improve the recovering processes in the treatment because through psychological intervention enabled clients to bring psychic stability, improvedthe recovering processes in the treatment because through psychological intervention enabled clients to bring psychic stability, improved a quality of life and coped with condition.
LITERATURE REVIEW
The management of psychological consequences to people diagnosed with cancer was very significant because oncology patients suffered with many psychological problems such as emotional liability, changes in future perspectives, feelings of loneliness, abandonment, stigmatization and interpersonal problems (Bras., 2008). The study done in Italycomments that most of international organizations dealing with cancer patients recommend that continuous monitoring of psychological distress in cancer patients throughout the disease were essential; the reasons for this concern was due to high frequency of psychological distress in cancer patients and it was associated with a worse quality of life, poor adherence to treatment, and stronger assistance needed (Muzzatti & Annunziata, 2011).
The study done in New York insists that the management of patients with cancer should include ensuring the psychological well-being of patients(Davies & D’Arcy, 2013). The holistic approach management to cancer patients during chemotherapy were needed because the range of depression, anxiety and stress was 90%, 56% and 28% (Singh & Banipal, 2017). The psychological management had been effective in reduced distress and improved overall quality of life among patients with cancer (Adler & Page, 2008). A cancer diagnosis caused distress to patient, to the partners, as well as family as a whole. The psychotherapy aimed to less distress and more relationship satisfaction for both the patient and partner (Manne, Ostroff, Norton et al., 2006) The psychological management of patients with cancer differ depending on the specific disorders; such as an adjustment disorder, an anxiety disorder, a depressed disorder, pain and fatigue (Holland & Alici, 2013). These interventions were experiential supportive for treating distress in cancer patients included supportive-expressive group psychotherapy (Classen, Kraemar, Blasey, et al., 2008).
Cognitive behavioral therapy (CBT) as one of the essential therapy involved the relaxing, enhancing problem solving skills and identifying and corrected an inaccurate through associated with feelings. It showed effectively reduced psychological symptoms (anxiety and depression) (Carr & McNulty, 2016) as well as physical symptoms (pain and fatigue) in patient with cancer (Johnson, Hopwood, Cesario et al., 2017). It is co-operated with mindfulness for stress management (Breitbart et al., 2015). The psychotherapeutic intervention in oncology benefits in reduced the severity of psychological or psychiatric symptoms as well as somatic symptoms and improved quality of life well-being; (Henningsen, 2018).
Psychoanalytical therapy viewed people as being significantly influenced by unconscious motivation, conflicts between impulses and prohibitions, defense mechanism and early childhood experiences (Corey, 2009). The psychologist who provide therapeutic services on oncology department should be familiar with psychoanalytic theory and concepts of psycho-sexual development because it contributes to an understood of unique personality to patients, the specific models of stress response, unique defense mechanisms, and memory as a result of unique experienced, fantasy, desire, dreams, thoughts and feelings (Neuburger, 2000). When patients with cancer experienced suffering due to disease they show several defense mechanisms such as denial, projection so to free himself from regrets provoked by disease. Also they show rationalization especially when avoided anxiety and loss and self-esteem. Psychotherapeutic approach is in worked with oncology patients based on defining personality structure of patients, current problems, and patient situations, included identifying life events and crisis that could affect current situation, defenses for reduced disease related stress, hospitalization, operative or conservative treatments and behavioral patterns used in the past as possible predictors of reactions to present situations. The aim of psychotherapeutic interventions during treatment of oncology patients was reduced and removed difficulties and bringing psychic stability (Gregurek, 2006). Psychological management approach in treating oncology patients contains worked with patients, from the beginning of diagnosis till the end of treatment as well as worked with the medical team (Neuburger, 2000).
The supportive psychotherapy is the cornerstone of emotional support for patients with cancer, additional, psycho-therapeutic interaction should be provided depending on the needs of the patient (Barlow, Durand & Hofmann, 2018). Supportive psychotherapy in groups showed improved quality of life and psychological symptoms especially improvement of mood and pain control in patients with cancer (Adler & Page, 2008) but the selections of intervention were done in relation to several variables including clinical psychological condition; the type and phase of illness and situation of the patient (Grassi, Johansen, Annunziata et al., 2013).
The existential therapy had provided further convinced evidence that discussion of death and meaning in life decreased rather than increased depression and improved quality of life (Spiege, 2015). These therapies (existential therapy) focus more on define the meaning of life (Kissene, Bloch, Smith et al, 2003). It challenged to accept our aloneness and created a meaningful existence; because we were basically free and aware (Corey, 2009).
Usually the outcome of untreated psychological issues in cancer recently had identified but simultaneous treatment of psychological issues including distress in cancer showed to improve outcome (Walker, 2013).The psychological distress affected functioning, capacity to cope, treatment compliance, quality of life and survival of patients with cancer (Portman, 2015) therefore was essential to provided intervention. For example; anxiety associated with cancer amplifies feelings of pain, interferes with sleep habits, caused nausea and vomiting, and negatively effects on patient’s quality of life (Stark & House, 2000). Unless it treated serious, anxiety can affect the length of patients’ life (Bras, 2009). The psychological distress needed a professional people such as psychologists because patients can have provided a verbal and non-verbal information about their emotional state; however, many may not have revealed emotional issues as they believed it was not a doctor’s role to help them with their emotional concerns. Patients may normalize their feelings; for examples anxiety and depression can mimic physical symptoms of cancer or treatments, and thus emotional distress may not notice and remain untreated (Ryan et al., 2005).
The main objective of this study is managing the psychological distress to people suffering with cancer. The counseling as the psychological management methods is important to resolving psychological distress to cancer patients (Ostovar et al., (2022) but there were limitation due to the fear of cancer patients that usually think that will get another cancer (NCI, 20202).
Not only that, but also, most of cancer patients in Sub-Sahara of Africa come to the hospital late which may limit early provision of psychological intervention to cancer patients (WHO, 2022). The higher prevalence of psychological distress were among the female and individual with lower income which usually delay to come to hospital for treatment (Kranenburg & Shen, 2023).
METHODOLOGY
Research Approach and Design
Research Approach
The study aimed to find out the management of psychological distress to cancer patients. The study used both quantitative and qualitative research approaches in order to gain a deeper and broader understanding. The qualitative approach was used in the interview for the purpose of getting detailed information and the quantitative approach used questionnaires to cancer patients for statistical data.
Research Design
Research design for this study was a cross sectional analytical hospital based study design that employed mixed methods (quantitative and qualitative) in order to maximize strength and minimize limitation of each approach as well as a method of collecting information by providing questionnaires and interviewed to sample of individuals. According to Bryman, (2008) cross-sectional design has placed it defined in the context of quantitative research, but it also should be noted that qualitative research often involves a form of cross-sectional design. A firmly typical form of such research is when the researcher employs semi-structured interviewing with a number of participants. The study took place at a single point and it involved looking data from a population at once at a specific point. In the current study the researcher looked data at a single and specific point, that was at KCMC to cancer patients as a targeted population.
In the present study semi-structured interview questions were used to obtain views, opinions about how to manage psychological distress in cancer patients. In this study a researcher administered questionnaires to get information about management of psychological distress to cancer patients.
Quantitative and qualitative data in this study were sought in order that variations variables can be systematically evaluated according to the specific and reliable standards(Walliman, 2007).
Description of Study Area
The study was conducted at KCMC, a zonal hospital in Moshi Municipality, Kilimanjaro Region situated in the North Eastern of Tanzania at the lower slope of Mount Kilimanjaro. In 2012 it was estimated to have a population of 184,292 people. Moshi Municipality covers about 59 square kilometers and it attained the status of a town in 1956 and in 1988 became a municipality. Moshi is one of the tourism centers in northern Tanzania. People in Moshi, apart from practicing tourism, they cultivate coffee, banana, beans and maize (Tanzania, 2013). KCMC was selected among the zonal hospitals which conduct clinics of cancer patients referred to from all regions of northern zone including Arusha, Tanga, and Manyara.
Population, Sample and Sampling Techniques
Target Population of the Study
The target population was cancer patients attending at the Cancer Care Centre at Kilimanjaro Christian Medical Center (KCMC). This included patients who were attending the clinic for consultations and treatment at the center. The study also included medical staff who were working in the Oncology Department during the study period.
Sample Size for Quantitative
The sample size of this study was approximate of 216 respondents, the 40% of the 540 of the respondents (cancer patients). During the study the 175 respondents were involved which were 41% of 427 respondents who attended. According to Sanga (2011), the range recommended for the sample size is 25 -30%. This helped to reduce sampling error which was reduced by increase of sample size.
Sample Size for Qualitative
The sample size of this study in qualitative comprised eight participants: the staff (Oncology Doctors and Nurses) working in the oncology department at KCMC. The participants were 45% of staffs in this department.
Sampling Techniques
Systematic sampling technique was employed to obtain 175 respondents and purposively sampling of eight participants. Attendance was portrayed on a paper list on each day of data collection. One of the staff on the desk was trained and instructed about the list provided; hence, she/he had all responsibilities of directing the patients to the respective desk for provision of questionnaires and consent.
Sampling Procedure
For quantitative methods, the 427 patients attended Cancer Care Centre at KCMC hospital. The adult was 403 and children were 24 who were excluded. The systematic random sampling was used thus every second person was selected to represent the participants in the study, therefore the 201 were not involved and 202 were involved. Out of 202 patients, five were very sick and 22 were new referral for consultation who was not yet diagnosed. The 175 respondents participated in the study.
For qualitative method, eight medical staffs (the oncology doctors and nurses) were selected using purposive sampling method for interview. The purposive sampling used because the information was provided to achieve objectives of this study.
Sources of Data
The sources of data in this study were primary and secondary.
Primary Data
The primary data are those data which were collected or obtained from participants and respondents of this study through questionnaires and interview.
Secondary Data
These are the facts that are recorded before a study is done. They come from various sources of the documents for the aim of supporting primary data which were used in the study especially in the discussion and recommendation. In this study, records from the oncology department at KCMC were used.
Methods of Data Collection
Interview Methods
Semi-structured interviews were used to some of participants; the staffs (oncology doctors and nurses) working in the Oncology Department. The open ended questions were prepared focusing to the research objective that intended to be covered concerning “Psychological Distress Management to Cancer Patients”. The present study was used interviews to get the detailed information about the psychological management to cancer patients who suffered with psychological distress.
Questionnaire
The information was collected through questionnaires from cancer patients. The questionnaire divided into two, eight demographic information questions and psychological intervention of three questions.
Validity and Reliability of Data Collection Instrument
Validity and Reliability in Quantitative
The validity shows the accuracy and truth of the data in research, while reliability means that if the research is repeated by the respondents with the same methods they will acquire the same results or data (Beck, McKeown &Kulan, 2015). For the purpose of achieving validity in the current study, questions were designed in such a way that they capture relevant information for the research objectives.
Reliability in Qualitative
Reliability in qualitative is a trustworthiness depending on coding scheme. The elements of trustworthiness in the research are credibility, transfer ability, dependability and conform ability (Bryman, 2008). In the present study, all these elements were maintained to have a standard of qualitative result of the study. The validity in qualitative should be measured as credibility, transfer ability, dependability and conform ability
Credibility
The credibility refers to confidence of the truth of the findings (Bryman, 2008). The current study established a confidence that the result from participants were true and believable by provided a consent forms, followed the interview protocol which allowed the participants to be familiar of the study.
Transfer ability
Transfer ability shows that the findings have applicability in other context, situations, times and population. The present study, the expressions of the participants were put into the context of the background problems of the research study framed.
Dependability
Dependability showing that the findings are the consistency of inquiring process used over time (Bryman, 2008). In the current study the logic used to select participants for interviews and data was clearly presented. The data of this study was audited and supervisor reviewed the activities done by researcher throughout.
Conform ability
The conformability is a degree of neutrality or the extent to which the findings of a study are shaped by the respondents and not a researcher bias motivation (Bryman, 2008). The present study, a researcher was neutral and free from bias in all process of qualitative data collection through the guided interview questions.
Data Presentation and Analysis
Data Presentation and Analysis of Quantitative
Data analysis is the process of examining what has been collected in the study by making deduction and inferences according to the objectives of the study (Kombo & Tromp, 2006). It is a brief of statement on the analysis and interpretation of data (Mlyuka, 2011). This study, the raw data were collected, organized, coding and put it into appropriate form. Entry, clearing and analysis of quantitative data were done through Statistical Package for Social Science (SPSS) version 20. Univariate and bivariate were used in the analysis of psychological distress management to cancer patients. The tables, figures, and percentages were used.
Data Presentation and Analysis for Qualitative
However thematic analysis of qualitative data obtained through the interview was used. The researcher took notes, recorded and transcribed the data for analysis. Organization of the ideas was done using codes in order to identify similar ideas hence identifying the merged themes which related with the study of the third objective. The information was put together in major themes. For instance, there were themes obtained from oncology doctors which were similar from oncology nurses during the interview.
Ethical Considerations
This study ensured the ethics; every participant was treated with respect and dignity; protected with harm and promote welfare of individuals. The permission from the University of Iringa was granted through the letter after defending the proposal of study. The request letter was written to KCMC, the institution where the study took place. Then kindly asked permission verbally and by the used of consent form for each participant was done. The participant was free to participate in the study or free not to participate. Naming of participants was not written on the statistical analysis.
RESULT
Management of Psychological Distress among Cancer Patients at KCMC
This is an objective of the study which analyzed using both quantitatively by used the SPSS 20 version and qualitatively used thematically. The quantitative findings consist 175 respondents who were provided with questionnaires, focus on management of psychological distress to cancer patients. The respondents were asked if they got any psychological treatment since they were diagnosed to have cancer.
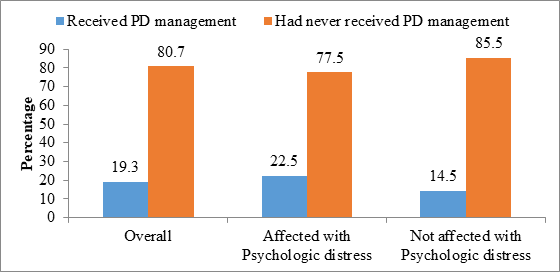
The respondents who replied were 171, and four did not answer this question. Out of the respondents who answered, 138 (80.7%) they did not receive psychological distress management since they had seen diagnosed as cancer patients; only 31 (19.3%) were getting psychological distress management. This study showed that 79 (77.5%) had never received psychological distress management, only 23 (22.5%) received psychological distress management.
Figure 1: Management of Psychological Distress among Cancer Patients at Kilimanjaro Christian Medical Center.
Source: Researcher, 2020.
Common Psychological Therapies to Cancer Patients with Psychological Distress:
The most common psychological therapies to cancer patients are cognitive behavioral therapy, psychoanalytical therapy, group supportive therapy and existential therapy. The respondents were asked to describe the type of psychological therapies they get.
Table 1: It describe psychological therapies the cancer patients they get
| Frequency | Percent | ||
| Valid | Cognitive behavioral therapy | 2 | 1.1 |
| Other therapy | 31 | 17.7 | |
| Total | 33 | 18.9 | |
| Missing/No | 131 | 74.9 | |
| System | 11 | 6.3 | |
| Total | 142 | 81.1 | |
| Total | 175 | 100.0 | |
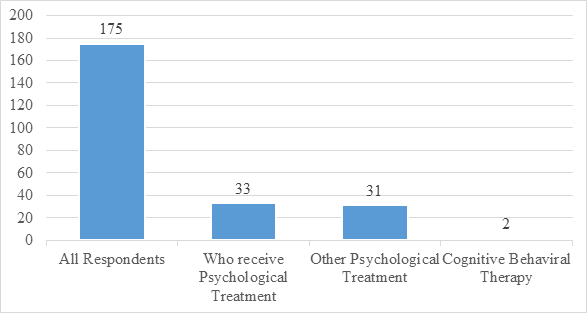
This question intended to find out which type of the psychological therapies the cancer patients get out of the common types including Cognitive Behavioral Therapy, Psychoanalytical Therapy, Supportive Group Therapy and Existential Therapy. This question was answered and out of the 175 respondents; only 33 respondents received psychological distress management and 142 (81.1%) did not answer that question (see table 4 above).
Out of 33 (25.3%) respondents who received psychological distress management, only 2 (6%) respondents had cognitive behavioral therapy and 31 (19.3%) received other management such as education about disease, encouragement and information giving about disease and side effect of medication (see the figure 2 below).
Figure 2: Common Psychological Therapies to Cancer Patients.
Source: Researcher, 2020
(NOTE: Y-Axis is Number of patients; X- Axis is Type of Psychotherapies)
According to the findings, most of the recognized psychological therapies for managing psychological distress (x-axis) such as psychoanalytical therapy, support group therapy and existential therapy were not practiced to cancer patients, only cognitive behavioral therapy was practiced but only by little 6 (2%) (Y-axis). More details regarding psychological distress management therapies offered to cancer patients have been narrated though qualitative approach results received after interviewing was done to eight staff (three oncology doctors and five oncology nurses) who treat cancer patients. The most common psychological therapies were interviewed, one by one as per subcategories.
The Qualitative Findings
A researcher was interested to get a detailed information about a third objective of the study which were about to determine the ways of managing psychological distress to cancer patients. The semi-structured questions were used to interview the eight participants (three doctors and five nurses) in this study and a researcher explored this detailed information through the following sub-categories.
Psychological Intervention for Cancer Patients
The researcher was interested to know about the types of the psychological interventions offered by oncology doctors and nurses to cancer patients. During the interview the participants were asked about the types of psychological treatment they offer to cancer patients. The second oncology doctor responded as follows.
Well…., somehow we do it; because we inform the patient about his or her illness, in order to agree about treatment which will be offered to him or her. Most of the patients with cancer experience fear, therefore after informing them, we give time to decide and agree with treatment (Doctor Two).
This finding showed that oncology doctors offering more information about illness, they do not provide psychological intervention for cancer patients. The aim of providing such information is to convince cancer patients to adhere the treatment offer in the oncology clinics. They agreed that cancer patients suffer with psychological problems such as fear.
Also the oncology nurse four responded that, “We offer psychological treatment by educating about illness, the causes and treatment of disease and side effect of medication” (Nurse Four).
From these two quotations above, the oncology doctors and nurses they misinterpreted the psychological interventions; and or lack of understanding about offering psychological intervention for cancer patients. This is because, once they educated about the illness, including causes, treatment and side effect of medication, think that, by doing so, they provide psychological intervention to patients. Also they were not aware about types of psychological intervention should be offered to cancer patients. Thus it shows that the need for doctors and nurses to learn psychological intervention skills.
Cognitive Behavioral Therapy to Cancer Patients
A researcher also wished to know the cancer patients who attend in the clinic if the oncology doctors and nurses provide the cognitive behavioral therapy as one of the psychological therapy. Through interview, to this subcategory, participants were asked to explain how they offer Cognitive Behavioral Therapy to cancer patients.
This is what nurse one said:
Aaaa …. Patients who are in the last stage develop false belief, that, the medication from hospital cannot help them anymore; therefore, they seek traditional medicine. As medical personnel we challenge their thoughts and belief about traditional medicine; then some of the patients (not all) agree and accept the hospital medication (Nurse one).
The findings reveal that when the patient are occupied by false belief or thoughts, which lead to resistance of using hospital medications, doctors and nurses try to challenge them instead of doing fully cognitive behavioral therapy, for the purpose of continue use of hospital medicine instead of using traditional medicine. This found to be difficult because it is not all patients adhere hospital medication.
Another participant respond by saying:
“Oooh …. It is true, our patients develop false belief and distorted thoughts about medication and think about traditional medications but as we start treatment to any new cancer patient we educate them about illness and this help to reduce fear” (Doctor Two).
Doctor agreed that cancer patients experienced false belief and distortion of thoughts, but what they do, they educate about illness which helps patients reduce fear but do not offer Cognitive Behavioral Therapy per say.
The response of the other two staffs were: “Yaa…. Our cancer patients are mentally disturbed; we real need Psychologist to counsel them” (Doctor One). “In our department we do not do this therapy” (Nurse five).
In these findings of two participants (doctor one and nurse five) observed that cancer patients their not psychic stable, they were mentally disturbed, thus need psychologist to address psychological problems and provide interventions because they do not do Cognitive Behavioral therapy.
Psychoanalytical Therapy to Cancer Patients
To this subcategory, a researcher was more concerned about psychoanalytical therapy to cancer patients and participants were asked to explain how they offered this therapy to cancer patients.
These were their responses;
“I have never treated a patient using this approach, and I don’t know this therapy, and I did not see any medical personnel using this therapy” (Nurse one). “Most of the time we do not explore enough the source of depression and anxiety by relating the traumatized past events of the patients” (Doctor two).
The data above shows that this type of therapy is not known to oncology doctors and nurses but for those who wishes to know better the source of the depression and anxiety due to traumatize events, they do not have enough time. That means they do not provide this therapy because they lack understanding and enough time to explore more about traumatized events relating to depression and anxiety.
Supportive Group Therapy to Cancer Patients
In this subcategory, researcher intended to find out if cancer patients who attend clinic get an opportunity to share their psychological concern (include anxiety, adjustment disorder and depression) in the groups therapy. In the interview, participants were asked to explain how they offered Supportive Group Therapy to cancer patients.
These were their responses:
Nurse three: “We talk to our patients and welcome them to share and witness to others about their good progress, and they have been living long life after been diagnosed as a cancer patient”. Doctor one: “The patients who are friends, we gather them together with a nurses and share their experiences. Patients receive information not only from medical personnel but also to their fellow patients who have good progress”.
According to these findings, oncology doctors and nurses offer the supportive group therapy to cancer patients by making a group to patients who were friends and those who had good progress and experience. The experienced patients who live a long time after being diagnosed with cancer witnessed to fellow patients and motivate them.
Existential Therapy to Cancer Patients
In this subcategory, the researcher interested to explore more about the psychological distress management through existential therapy. The participants were asked to explain how they offered existential therapy to cancer patients. In the interview, doctor three were responded by saying that “We do a little to our patients through counseling and ensuring about their life” (Doctor three). Another participant comment that “We provide this therapy by involving pastors to talk with our patients the Word of God for comfort” (Nurse three).Regarding these two responses, the oncology doctors and nurses, most of the time, were not in the position to offer this therapy but used spiritual leaders to discuss the Word of God with cancer patients for comfort and describe about the meaning of life to cancer patients.
The Outcome to Cancer Patients Who Receive Psychological Intervention
Furthermore, the researcher wanted to know more about the outcome of cancer patients who received information about illness, treatments and side effect of medication as a part of counseling they were receiving from oncology doctors and nurses. The participants were asked to explain the outcome to cancer patients who receive Psychological intervention.
These were their answers:
“I learnt that those who get counseling they progress well, use medication, attending the clinics they accept hospital treatment and neither despair nor use traditional medicine” (Doctor two).
“Those who receive counseling they progress very well, because they witness to others on how they recover due to the advice, counseling and education they got from us as a medical personnel” (Nurse Two).
According to the findings, it seems that those who get counseling services based on giving information about illness, treatments and side effects of medication, adhere to hospital treatment and become ambassadors to other cancer patients by sharing with them about their good progress.
Outcome to Patients Who Do Not Receive Psychological Intervention
The cancer patients in the questionnaire were asked about their progress although they do not get psychological intervention so to quantify or measure the outcome of the psychological distress in the following categories.
a) If patients were able to cope with distress although they did not receive psychological intervention.
Table 2: The Cancer Patients who were Able to Cope with Distress
| Frequency | Percent | ||
| Valid | No | 29 | 16.6 |
| Yes | 119 | 68.0 | |
| Total | 148 | 84.6 | |
| Missing/No | 27 | 15.4 | |
| Total | 175 | 100.0 | |
Source: Researcher, 2020.
The cancer patients who did not receive psychological distress management and were able to cope with distress in their life were 119 (68.0%), and those who failed to cope with distress were 29 (16.6%); but 27 (15.4%) did not respond to the question. (See Table 5 above)
b) If patients were able to comply with treatment they were receiving from hospital although they did not receive psychological intervention.
Table 3: The Cancer Patients who were Able to Complied with Treatment
| Frequency | Percent | ||
| Valid | No | 9 | 5.1 |
| Yes | 142 | 81.1 | |
| Total | 151 | 86.3 | |
| Missing/No | 24 | 13.7 | |
| Total | 175 | 100.0 | |
Source: Researcher 2020.
According to the findings, 142 (81.1%) were able to comply with treatment they received, although they did not get psychological treatment. The 24 (13.7%) missed to answer the question. The cancer patient who struggled for treatment compliance were 9 (5.1%). (See Table 3 above).
c) If they were able to manage their activities of their daily life although they did not receive psychological intervention.
Table 4: Cancer Patients who were Able to Manage Their Activities of Their Daily Lives
| Frequency | Percent | ||
| Valid | No | 91 | 52.0 |
| Yes | 57 | 32.6 | |
| Total | 148 | 84.6 | |
| Missing/No | 27 | 15.4 | |
| Total | 175 | 100.0 | |
Source: Researcher, 2020.
Regarding this finding, the respondents failed to manage their activities of daily living 91 (52.0%) those who do not get psychological distress management, since they were diagnosed as cancer patients. Those who managed their daily activities were 57 (32.6%). The respondents who missed to answer this question were 27 (15.4%). (See Table 4)
d) If they still experienced anxiety because majority did not receive psychological intervention.
Table 5: The Cancer Patients who Still Experienced Anxiety
| Frequency | Percent | ||
| Valid | No | 100 | 57.1 |
| Yes | 52 | 29.7 | |
| Total | 152 | 86.9 | |
| Missing/No | 23 | 13.1 | |
| Total | 175 | 100.0 | |
Source: Researcher, 2020.
The following were the responses of the cancer patients when were asked this question. It was noted that 100 (57.1 %) did not experience anxiety, but 52 (29.7%) experienced anxiety because of lack of psychological distress management. Twenty three (13.1%) did not answer the question. (See Table 5)
e) If they still experienced negative thoughts/feelings because did not receive psychological intervention.
Table 6: The Cancer Patients who Still Experienced Negative Thoughts/Feelings
| Frequency | Percent | ||
| Valid | No | 116 | 66.3 |
| Yes | 35 | 20.0 | |
| Total | 151 | 86.3 | |
| Missing/NA | 99 | 24 | 13.7 |
| Total | 175 | 100.0 | |
Source: Researcher, 2020.
The answers to the question above were 116 (66.3%) respondents did not experience negative thoughts and feelings, but, about 35 (20.0%) experienced negative thoughts due to lack of psychological distress since they were diagnosed to have cancer in their life and 24 (13.7%) missed. (See Table 6 above).
The researcher was also interested to know detail on what are their contribution as an oncology doctors and nurses about the outcome for cancer patients who did not receive the counseling and information of illness, treatment and side effect of medication. Through the interview the participants were asked to explain the progress of cancer patients who did not receive psychological intervention.
One of the doctors, said that: Most of the time, patients who were not counseled remain frustrated and with negative thoughts” (Doctor three).
Another participant respond that:
Okay…. Patients who do not understand the importance of counseling and ignore, they develop false belief about treatment and stop hospital medication and start the use of traditional medicine; then later come to the hospital with worse situation, they end up with poor progress(Nurse two).
The two quotations above imply that the cancer patients who remain without any counseling, and proper information about diseases, suffers with psychological problem include frustration, negative thoughts and feelings, develop false belief and left hospital medication and started using traditional medication. These result poor progression and worse situation to cancer patients.
DISCUSSION
Determine the ways of Managing Psychological Distress to Cancer Patients
Focusing on management of psychological distress to cancer patients. The findings of this study found less practices of psychological distress management of cancer patients, whereas about 6% of patients suffering from psychological distress get treated psychologically. Nevertheless, the methods for psychological distress management were not applied by health workers and this indicates possible worse conditions to patients suffering from psychological distress. The findings of the study by Ryan et al (2005) and Ma et al (2013) showed that psychological distress is often unrecognized and untreated to patients with cancer by clinicians. In this study, the findings in discussion with the clinical staff (doctors and nurses), it was observed that staff were lacking knowledge on psychological distress management that limit them from giving this potential treatment to patients because is not their professional. Doctors raised their concern that majority of cancer patients were suffering from psychological problem that cause some patients refuse to take medication and which resulted in more burden to their life including early death. However, they usually practice counseling to patients at their best level to make them accept the medication and continue with care.
The major reason for not giving psychological management is an absence of psychological counselors at the facilities or and it is not their profession to provide effective care for patients with psychological problem. This finding is contradictory to a study in the USA which showed that patients with cancer should be well managed for psychological well-being from the beginning of diagnosis to the end (Davies & D’Arcy, 2013). Another finding from the study in Italy found effective psychological distress management to cancer patients is essential by continuous doing and monitoring of psychological distress in cancer patients throughout the disease (Muzzatti & Annunziata, 2011).
The findings of this study showed that; most of the recognized psychological therapies for managing psychological distress to cancer patients (psychoanalytical therapy, supportive group therapy and existential therapy) were not practiced because is not the role of their doctors and nurses, but also they do not have professional psychological counselors in oncology department. Through interview, one of the nurse comment that: “I have never treated a patient using this approach, and I don’t know this therapy, and I did not see any medical personnel using this therapy” (Nurse one). She commented so when asked if they offer psychoanalytical therapy to cancer patients. This finding is contrary to the study done by Grassi, et al (2013) that commented that selections of psychological intervention therapies are virtual important depending on clinical psychological condition; the type and phase of illness and situation of the patient (Grassi, Johansen, Annunziata et al., 2013).
The findings of this study showed that, the cancer patients who get counseling most of them progress well. Two participants commented that:
“I learnt that those who get counseling they progress well, use medication, attending the clinics they agree a hospital treatment and neither despair nor use traditional medicine” (Doctor two).
The second participant commented that: “Those who receive counseling they progress very well, because they witness to others on how they recover due to the advice, counseling and education they get from us as a medical personnel” (Nurse Two).
Therefore, counseling, as a part of psychological intervention to clients are important to most of patients who experienced psychological distress because of illness including cancer.
The study findings showed that cancer patients who do not receive psychological distress management they experienced anxiety 52 (29.7%), depression 47 (26.9%) and difficult to compline with hospital treatment 9 (5.1%). Furthermore, cancer patients, who did not receive psychological intervention remain with negative thoughts/feelings 35 (20.0%) failed to cope with distress 29 (16.6%) in their life and majority find difficult to manage daily activities 91 (52.0%). The study findings correspond with the comment of Portman, (2015) who asserted, the psychological distress affected functioning, capacity to cope, treatment compliance, quality of life and survival of patients with cancer. Also one of the participants commented that “Most of the time, patients remain frustrated and with negative thoughts” (Doctor three). Therefore, what we see in the findings of this study is the same with the comment of the Portman, thus the psychologist for intervention are essential to cancer patients.
CONCLUSION
Psychological distress among cancer patients was high among cancer patients at KCMC which require management. The anxiety and depression were among the psychological distress disturbing even process of recovering among cancer patients. Marital status divorce, low income and low education status were significantly associated with psychological distress with less psychological management at the site.
RECOMMENDATION
First, the hospital administration has to allocate psychological counselors to Oncology Department to address psychological problems to cancer patients.
Second, Oncology Department should develop interest of doing research on managing psychological distress so to find an appropriate psychological approach for intervention for cancer patients according to their uniqueness.
Third, Hospital management should sensitize the protocol on the use different psychological therapies according to the psychological problem found in cancer patients
Fourth, Psychological issues with patients is an essential part to be explored and addressed among the patients and managed.
Lastly, further studies should be conducted in the hospital setting in order to discover more needs of our patients and improve our services to them
ACKNOWLWDGEMENTS
The supervisors and all participants who offered their time to participate this study.
RESEARCH ETHICS
Ethical approval was obtain from the faculty of psychology; Iringa University.
CONSENT
All participants provided an informed consent to participate in the study.
REFERNCE
- Aass, N., Fossa, S. D., Dahl, A. A., Moe, T. J. (2004). Prevelance of Depression with Cancer. Volume 2004. https://dio.org/10.1093/jncimonographs/lgh 014.
- Adler N. E & Page A. E . (2008). Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. Washington D.C: National Academic Press.
- Akter, J., Khan, J. G., Khan, M. H., Hossain, M. Z. (2015). Psychological Distress in Cancer Patients with underage Children. Middle East Journal of Cancer 24(2) 146-151
- Andersen, B. L., DeRubeis, R. J., Berman, B. S., Gruman, J., Champion, V. L., Massie, M. J., Holland, J. C., Partridge, A. H., Bak, K., Somerfield, M. R., and Rowland, J.H. (2014). Screening, Assessment and Care of Anxiety and Depression Symptoms in Adult with Cancer: An American Society of Clinical Oncology guideline Adaptation. Journal of Clinical Oncology.32: 1605-1619.
- Barlow D. H., Durand V. M., & Hofmann S. (2018). Abnormal Psychology: An Intergrative Approach. Boston: Nelson Educated Ltd.
- Beck I. L., McKeown M. G. & Kulan L. (2015). Bringing Word to Life Robust Vocabulary Introction. New York: Gulford Press.
- Boyle, P. & Levin, B. (2008). World Cancer Report.International Agency for Research on Cancer (IARC), Geneva, 1-6-2010.
- Bras, M. (2009). Antidepresive U lijecenjukronicreboli Onkologijiipalijativnojmedicini. Zegreb Medicinskanaklada Vol 7., 108 – 125
- Bras, M. (2008). Antidepresive U lijecenjukronicreboli Onkologiji ipalijativnojmedicini. Zegreb Medicinskanaklada Vol. 2., 1-32
- Bray, F., Ren, J., Masuyer, E., Ferlay, J. (2008). Global estimates of Cancer Prevalence for 27 sites in the Adult Population in 2008. International Journal of Cancer. 132 (5) 1133-1145
- Breitbart, W., Rosenfeld, B., Ressin, H., Applebaum, A., Kulikowshi, J., Lichtenthal, W. (2015). Meaning-centered Group Psychotherapy: An Effective Intervention for improving Pyschological well-being in Patients with Advanced Cancer, Journal of Clinical Oncology, 33 (7) 749-754
- Brighi, N., Balducci, L., & Biasco, G. (2014). Cancer in Elderly: Is it time for Paliative Care in Geriatric Oncology?Jounal of Geriatric Oncology, 5 (2) 197-203
- Bryman, A. (2008). Social Research Methods: New York: Oxford University Press Inc.,
- Carr A. & McNulty M. (2016). The Handbook of Adult Clinical Psychology: An Evidence Based Practice Approach . New York: Guilford Press.
- Classen, C. C., Kraemar, H. C., Blasey, C., Giese-Davis, J., Koopman, C., Palesh, O. G., Atkinson, A., DiMiceli, S., Stonisch-Riggs, G.,Westendorp, J., Morrow, G. R., Spiege, D. (2008). Supportive-Expressive Group Therapy for Primary Breast Cancer Patients: A Randomized Prospective Multicenter Tried. Free PMC Article. 17 (5) 438-447
- Comer R. J. (1995). Abnormal Psychology. New York: W.H Freeman & Company.
- Corey G. (2009). Theory & Practice of Counseling & Psychotherapy . Belmont: Thomson Brooks/Cole.
- Davies P. S., & D’Arcy Y. (2013). Compact Clinical Guide to Cancer Pain Management: An Evidence Based Approach for Nurses. New York: Springer Publishing Company.
- Ferlay, J., Soerjomatanam, I., Dikshit, R.., Eser S., Mathers C., Rebelo M., Parkin D. M., Forman D., Bray F. (2012) Cancer Incidence, Mortality and Prevalence Worldwide. International Journal of Cancer, 136 (5) E359-86.
- Gao, W., Bennett, M., Stark, D., Murray, S. (2010). Psychological Distress in cancer from Survivorship to end of Life Care: Prevalence Associated Factors and Clinical Implication . Europe Journal of Cancer, 46 (11) 2036-44
- Grassi, L., Johansen, C., Annunziata, M. A., Capovilla, E., Costantini, A., Gritti, P., Torta, R., & Bellani, M. (2013). Screening for Distressin Cancer Patients. American Cancer Society Journals, 119 (9) 1714-1721
- Gregurek, R., Bras, M., Dordevic, V., Ratkovic, A. S., & Brajkovic, L. (2006). Medicinska naklada – Zagreb Crotia: Psychiatric Danubina 2010 Vol 22, No. 2 pp. 227-230
- Gruneir, A., Smith, T.F. (2005). Depression in Patients Adviced Illness: An examination of Ontario Complex Continuing Care Using Minimum Date Set 2.0 Palliate Supportive Care. Doi 10. 1017/S1478981505050170
- Gundelach, A. & Henry, B. (2016). Cancer-related Psychological Distress: A Concept Analysis. Clinical Journal of Oncology Nursing, 20; 630-634.
- Henningsen, P. (2018). Management of Somatic Symptoms.Dialogues Clinical Neuroscience Jounal. Vol 20. No. 1
- Hoffe, S. & Balducci, L. (2012). Cancer and Age: Geriatric Consideration. Journal ofClinical Geriatric Medicine. 28 (1) 1-18
- Holland, J. C. & Alici, Y. (2010). Management of Distress in Cancer Patients . Journal of Support Oncology. 8 (1) 4-12
- Holland, J. C. & Alici, Y. (2013). Management of Distress in Cancer Patients. Journal of Support Oncology.8 (1)13-14
- Johnson D. J., Hopwood C., Cesario J., & Pleskac T. J. (2017). Advancing Research on Cognitive Processes in Social and Personality Psychology: A Hierarchical Drift Diffusion Model Primer. Research Article 8 (4): 1-11.
- Kamen, C., Mustian, K., Heckler, C. & Janelsins, M. (2015). Association between partner support and psychological distress among prostate cancer survivors. Journal of Cancer Survivorship 9 (3).
- Kapinga O. S. (2017). Cancer Statistic. Journal for Clinicians.
- Kissene, D. W., Bloch, S., Smith, G. C., Miach, P., Clarke, D. M., Ikin, J., Love, A., Ranieri, N. & McKenzie, D. (2003). Cognitive-Existential Group Psychotherapy for Women with Primary Breast Cancer: A Randomised Controlled Trial. Pscho-Oncology, 12 (6) 532-546
- Kombo, D. K. & Tromp D. L. A. (2006). Proposal and Thesis Writing: An Introduction. Nairobi: Publication of Africa.
- Komen, S.G. (2017). Tanzania Breast Health Care Assessment: An Assessement of breast Cancer Early Detection, Diagnosis and treatment in Tanzania. breast cancer foundation. GLOBOCAN 2012. International Agency for research on cancer 145 (1); 177-183.
- Kranenburg, L & Shen N. (2023). The Impact of Psychological Distress on Quality of care and Access to Mental Health Services in Cancer Survivors.
- Kumar R. (2005). Research Methodology a Step-by-step Guide for Beginners. Chicago: Sage Publication.
- Larkin, D.H. (2022). Cancer Deaths May Double by 2030 in Sub-Sahara Africa.
- Ma, L., Poulin, P., Feldstain, A., & Chasen, M.R. (2013). The Association between Malnutrition and Psychological Disteress in Patients with Advanced head-and-neck Cancer. Current Oncology, 20 (6), 554 – 560.
- Makofare, B., & Oyedeni, T. (2015). Parental Communication about sex and motherhood trends among Students at a South African University. Journal of University of the free State 20 (2015) 159-180
- Manne, S. L., Ostroff, J. S., Norton, T. R., Fox, K., Goldstain, L. & Grana, G. (2006). Cancer-related relationship Communicationin Couple Coping with Early Stage Breast Cancer. Journal of the Psychological, Social and Behavioral Dimensions of Cancer, 15 (3) 234-247
- Mason, A., Juyal, R.,Shikha, D., Das, S. C., Saini, S., & Semwal, J. (2019). Prevalence an Correlates of Psychological Distress among Cancer Patients in a Tertiary Care Hospital in Northern India. International Journal of Community Medicine and Public Health. 6 (5) 2223-2228.
- McFarland, D. C. & Holland, J. C. (2016). The Manangement of Psychological Issues in Oncology. Journal Clinical Advanced in Hematology Oncology. 14 (12) 999-1009.
- Mlyuka E. E. (2011). A Simplified Guide to Research Proposal and Report Writing for Institution of Higher Learning. Dar Es Salaam: Inter-Press of Tanzania Ltd.
- Muzzatti, B. & Annunziata, M. A. (2012). Psychological Distress Screening in Cancer Patients: Psychometric Properties of Tools Available in Italy. SAGE journals, 98 (4) 501-509
- NCI (National Cancer Institute), (2020). Helping Cancer Survivors Cope with Cancer-related Anxiety and Distress.
- Neuburger, R.P. (2000). Integration of a Psychoanalytic Liaison Department at a Public Hospital. Psychiatry Clinical Neurosci, 54: 399-406.
- Nuhu, F. T, Odejide, O. A, Adebayo, K. O., & Yusuf, A. J. (2009). Psychological and physical Effect of Pain on Cancer Patients. Article in African Jounal of Psychiatric DOI:10.4314/ajpsy. Vol. 10: 1211.30281.
- Ojewole, F. O., Madu, A. M. & Nwozichi, C. U. (2018). Association between Pyschological Distress and Unmet information Needs Among Female Cancer Patients in Two Selected Teaching Hospitals in South-west Nigeria. CHRSMED Journal of Health and Research. Vol. 5: 11-70
- Ostorar, S, Chahardeki, A, Hashim I.H.M, Othnan,A, Kvuk J & Griffiths M.D, (2022 ) Prevalence of Psychological Distress among Cancer Patients in Southeast Asia Countries: A systematic Review.
- Pirl, W., Fann, J. R., Greer, J. A., Brann, I., Deshields, T., Fulcher, C., Harvey, E., Holland, J., Kennedy, V., Lazenby, M., Wagner L., Underhill, M., Walker, D. K., Zabora, J., Zebrak, B. & Bardwell, W.A. (2014). Recommendation for the Implementation of Distress Screening Proframs in Cancer Center: Report from the American Psychosocial Oncology Society (APOS), Association of Oncology Social Work (AOSW),and Oncology Nursing (ONS) joint task force. American Cancer Society Journals 120 (19): 2946-2954.
- Portman. (2015, February ). Retrieved from National Comprehensive Cancer Network (NCCN) Clinical Practical Guidelines in Oncology: Distress Manangement: htt//www:nccn.org/professional/physician
- Prout H.T. & Brown D. T. (2007). Counseling and psychotherapy with Children and Adolescents: Theory & Practice for School and Clinical Settings. New Jersey: John Wiley & Sons Inc.,..
- Ridner, S. .H. (2004). Psychological Distress: Concept analysis. Journal of clinical Nursing, 45 (5): 536-545.
- Ryan, H., Schofield, P., Cockburn, J., Butow, P., Tattersak, M., Turner, J.,Girgis, A., Bandaranayake, D. & Browman, D. (2005). How to recognize and Manage Psychological Distress in Cancer Patients. European Journal of Cancer.14; 7-15
- Siegel, R., Naishadhan, D. & Jemal, A. (2013). Cancer Statistics. Cancer Journal for Clinitians, 11 – 30.
- Siege, R, Miller, K, Wagle, N, & Jemal, A (2023). A Cancer Statistic.
- Singh, H. & Banipal, R. (2017). Psychological Distress in Cancer Patient during Chemotherapy: A cross-sectional Study. Jounal of Clinical Oncology. Oncology 34 no. 26-supply
- Spiege, D. (2015). Existential Psychotherapy for Patients with Advanced Cancer: Facing the Further and the Past . Journal of Clinical Oncology 33, no. 24 pp 2713-2714
- Srikanthan, A., Leung, B., Shokooki, A., Smrke, A., Bates, A., & Ho, C. (2019). Psychosocial Distress Score and Needs among newly Diagnosed Sarcoma Patients: A Provincial Experience. Research Article. Volume 2019, https://doi.org/10.1155/2019/53026639
- Tanzania. (2013). 2012 Population and Housing Census: Population Distribution by Administrative Areas. Dar Es Salaam: URT-Population and housing Census.
- Uwayezu, G.M., Gishoma, D., Sego, R., Mukeshimana, M., & Collin A. (2019). Anxiety and depression among cancer patients: Prespective association factors at a Rwandan Referral Hospitals . Rwanda Jounal of medicine and Health Science. 2(2) 118-125.
- WHO (2014). Comprehensive Cervical Cancer Control: A guide to essential practice . World Health Organization, Geneva
- WHO (2022). Cancer . Annual Report of Cancer .World Health Organization, Geneva
- Walliman. N. (2007). Research Methodology: The Basics. London: Taylor & Francis Press.
- Zabora, J., Brintzenhofeszoc, K., Curbow, B., Hooker, C. & Piantadosis, S. (2001). The Prevalence of psychological distress by Cancer Site. Psycho-Oncology Jounal 10: 19-28 (2001) Baltimore: John Wiley & Sons Ltd.