A Study of the Factors Affecting Dental Community Health in a Multicultural Immigrant Educational Environment. A Systematic Review of the Recent Scientific Articles.
- Theodorou Andreas
- Koufioti Georgia
- Kounios Athanasios
- Dr.Vlachadi Maria
- 278-297
- Apr 28, 2023
- Public Health
A Study of the Factors Affecting Dental Community Health in a Multicultural Immigrant Educational Environment. A Systematic Review of the Recent Scientific Articles.
Theodorou Andreas1*, Koufioti Georgia2, Kounios Athanasios3, and Dr. Vlachadi Maria4
1Dental Laboratory Technician & Educator in Dental Technology, MSc, University of Nicosia, Nicosia, Cyprus
2Political Scientist, MSc, International Hellenic University, Kavala, Greece
3Manager of Healthcare Organizations, MSc, International Hellenic University, Kavala, Greece
4 Lecturer, PhD, Department of Political Science, University of Crete, Crete, Greece
DOI: https://doi.org/10.47772/IJRISS.2023.7422
Received: 26 February 2023; Accepted: 27 March 2023; Published: 28 April 2023
ABSTRACT
Introduction: Oral health is part of the broader context of health. Oral health inequalities directly affect groups that have endured and continue to face racism and injustice. Immigrant communities have higher rates of caries and tooth loss and lower rates of annual dental visits. Oral health interacts and affects multiple chronic health conditions. The purpose of this study is to initially conduct systematic research into the quality of immigrants’ dental health.
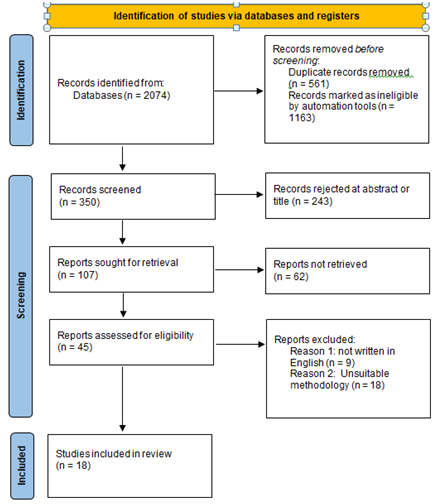
Methodology: A systematic review was performed using the PRISMA flow chart. The chronological range was set at 2010-2020.
Results / Findings: Changes in social life after migration play a critical role in the health of migrants and ethnic minorities, including their oral health. Immigrants and ethnic minorities experiencing social support either from their immediate environment (eg family members and friends) or from the wider community have had increased use of dental care and improved oral health, including caries and periodontitis. disease. In addition, social support had a positive effect on oral health self-assessment and on the quality of life associated with oral health. Immigrants and ethnic minorities with strong social ties also had more knowledge about oral health and oral care.
Conclusions: Several current emerging threats and risks exposing public health vulnerabilities are linked to global processes such as the economy, trade, transport, the environment and climate change, and political security. International migration, which is a supporting element and consequence of globalization, is increasingly affecting the health of countries of origin, transit and reception of migrants.
Keywords: Migration, Oral health, Dental care
INTRODUCTION
The broader context of health includes oral health. Disparities in oral health have a direct impact on racial and social groups that have experienced and still experience racism and injustice. Communities of immigrants have lower rates of yearly dental appointments and greater rates of tooth decay and tooth loss.
These disparities have immediate repercussions. Numerous chronic health issues interact with and are impacted by oral health. Patients with inadequate oral health needs frequently wind up in hospital emergency departments, where their dental illnesses cannot be addressed in a timely manner. This results in serious implications for the patients themselves as well as enormous financial burdens on the healthcare system.(Adibi et al., 2020).
According to the International Organization for Migration (IOM), a migrant is any person who moves or has moved across an international border or within a state away from his or her usual place of residence, regardless of the following factors: (1) the person’s legal status; (2) whether the movement is voluntary or involuntary; (3) the reasons for the move; (4) the length of the stay (Farmaki & Christou, 2019; Shevchenko, 2020).
With 22.3 million migrants residing in the EU, they are now performing a more significant role in European society (Pelizza, 2020; Reher & Requena, 2009). The concept of migration itself, however, is not without its difficulties. Migrants’ quality of life, which includes their dental health, might be significantly impacted by adjusting to the social, economic, and psychosocial factors of the migrant phenomenon (Batra et al., 2019). It is obvious that the consequences of poor dental health among immigrants are frequently cited as a crucial issue in research and decision-making (Skeie et al., 2006).
It has typically been noted that immigrants from low- and middle-income regions are more likely to have a prevalence of poor oral health when they immigrate to high-income countries such as the USA, Canada, Australia, and Europe (Dahlan et al., 2019; Gao, 2011; Scholten et al., 2015; Wickramage et al., 2018). For instance, a systematic study revealed that South Asian immigrants reported poor oral health knowledge, attitudes, and behaviors, which were primarily influenced by culture, social norms, and religion (Batra et al., 2019). Another study found that immigrants reported poorer oral health habits than the host community, brushing their teeth less frequently and consuming more sugar on average (Skeie et al., 2006).
Dental health has been recognized as a priority health indicator for 2020 due to the significant interaction between oral and general health. Oral inflammation (the management of oral disorders) can be quite expensive, both for the patient and for the healthcare systems because they are common and recurrent (Jin et al., 2016). Between 2008 and 2012, the European Union (EU) invested €79 billion on dental care; in 2020, that amount is projected to increase to €93 billion (Patel, 2017). Additionally, it has been demonstrated that having poor dental health might reduce quality of life (Ferreira et al., 2017).
According to studies on the dental health of Americans, people from specific ethnic minorities frequently have poor oral health(Hunt et al., 1995; Satcher, 2017; Watt & Sheiham, 1999). Ethnic minorities are not always associated with poor dental health. It does, however, imply that there might be some cultural practices and attitudes that people in these groups share that affect their oral health status, such as expectations for preventive or therapeutic interventions or values about providing healthy teeth. Cultural variables can have a significant impact on an individual’s health as well as the health of those they care for, such as children and the elderly (Hilton et al., 2007; Milnes, 1996; Riedy et al., 2001).
Ethnic minorities account for a growing share of the general population in the UK. In the UK, non-white groups comprised 13% of the population as per the 2011 Census. Only 46% of the population in London, the city with the greatest ethnic diversity in the UK, was identified as “White British” in the most recent census. In order to comprehend the general and oral health of the population and to develop suitable, responsive services, it is crucial to grasp country variances. However, in comparison to the extensive literature on socioeconomic disparities in oral health and access to dental treatments, ethnic differences in oral health have been largely ignored(Steele et al., 2015).
The World Health Organization has lately identified sugar consumption as a significant public health issue and a common risk factor for many chronic diseases (Organization World Health, 2015). Sugar consumption, which is present in sweets, meals, some medications, and carbonated soft drinks(Vartanian et al., 2007), predisposes enamel to demineralization and, as a result, causes caries to develop. Periodontitis is carried on by insufficient plaque control and is also significantly worse by smoking(Klinge & Norlund, 2005)as well as new risk factors such alcohol consumption(Tezal et al., 2004)and nutritional inadequacies(van der Putten et al., 2009). It is recognized that lifestyle risk factors, such as smoking and dietary sugar, vary by ethnic group (Leung & Stanner, 2011).
The two main conditions that lead to tooth loss and have been repeatedly linked to poor health are uncontrolled caries and periodontal disease(Klinge & Norlund, 2005). Good general health and a high quality of life depend on having good oral health. Pain and difficulty speaking or eating due to poor oral health can affect daily life, including work(Petersen et al., 2005). The social economic burden is also considerable because, in high-income nations, the cost of treating oral disorders ranges from 5 to 10 percent of the budget for health services(Petersen, 2003).
The research’s initial objective is to conduct a thorough assessment on the quality of immigrants’ oral health, available prevention and problem-solving programs, and potential educational approaches for use in immigrant integration centers and hotspots.
METHODS
The research’s first goal is to examine the dental health status of refugees and immigrants using pertinent literature, and the research issues that arise as a result of the subsequent bibliographic evaluation. The recording of initiatives that support the prevention and treatment of any dental health issues in the immigrant-refugee population raises another research subject.
An attempt is made to include all original studies that address one or more of the three oral health endpoints in this systematic review, including self-reported or clinically evaluated oral health status (dental caries, periodontal disease, oral cancer, orthodontic problem), self-reported oral health behaviors (tooth brushing, fluoride use, sugar consumption, nutritionpractices, tobacco and alcohol consumption), and/or oral health use (dental follow-up/barriers faced). Originally, the research on immigrants residing in Europe was the only study included; however, due to a dearth of papers and relevant research, the systematic review also included studies on immigrants living in other continents.
Methodologically, all studies that used terminology like minority groups, ethnic groups, immigrants, minority ethnic groups, or studies relating to a single ethnic group such South Asian, Chinese, Turkish, Moroccan, or Eastern European were included. A significant drawback of the study is that it only included studies that were published between 2010 and 2021, limiting the possibility of generational comparisons between immigrant groups when assessing the oral health status of current European immigrant groups.
The exclusion criteria included reviews, clinical case studies, case reports, and other non-research studies. Studies on refugees, asylum seekers, or undocumented immigrants were also excluded because they lay under a different set of circumstances than the general immigrant population.
The study procedure adhered to the PRISMA criteria for “Reporting of Systematic Reviews and Meta-Analyses.”(Liberati et al., 2009). Using the online literature databases Core and PubMed, a thorough search up to 2021 was conducted. In English, search terms included “immigrants,” “ethnic groups,” “immigration,” “social support,” “social network,” “social relations,” “social inclusion,” “social connection,” and “social bond.” Other search terms included “periodontitis,” “dental diseases,” “dental caries,” periodontal disease, “dental diseases,” and “dental diseases.” In the first stage, the titles and abstracts of the papers were examined to determine which ones were pertinent. After that, the abstracts and full texts were assessed using the inclusion criteria. The same search terms were also used in a grey literature search in Google Scholar and the Google search engine. Duplicate results were eliminated and search results were exported to Mendeley.
Four categories were used to retrieve data from the selected studies:
1) The study’s general characteristics, including its purpose, reported nationality or immigration, sampling strategy, sample size, age distribution of the target population, and study design;
2) Oral health outcomes: self-reported oral health status through surveys or interviews, reported oral health status using clinical indicators;
3) Oral health practices: habits including smoking, drinking alcohol, using fluoride, and cleaning the teeth are all behaviors that can be documented through surveys or interviews.
4) Use of oral health services: dental checkups or follow-up appointments, the type of dental work received, and any impediments, if any.
The following pre-determined inclusion criteria were thus met by cross-sectional and longitudinal quantitative and qualitative research that were included:
1) Researching links between social support and at least one oral health issue (such dental caries, periodontal disease, self-reported oral pain, denture issues, painful or bleeding gums, or dry mouth) or oral health behavior (such as dental care use, brushing, flossing the diet)
2) included an evaluation tool for oral health status or behaviors and a well-defined measure of social support.
3) were carried out with at least one ethnic or immigrant group.
The study omitted editorial pieces, conference abstracts, and literature reviews. There were no limits based on socioeconomic position, gender, or age.
RESULTS
The PRISMA flow chart is presented in Figure 1, followed by Table 1 with the summary of the studies included in the systematic review.
Figure 1. Presentation of PRISMA Flow Chart results
Table 1. Summary of studies included in the systematic review
| Authors | Country | Methods | Participants and age | Purpose | Main results |
| Brzoska, et al. (2017) | Germany | Telephone survey via questionnaire | No. 41,220
Age. >18 |
Examining the impact of demographic, social, behavioral, and health factors on immigrants and non-immigrants living in Germany was the goal of the study. | Lower odds of using routine dental exams were connected with younger age, being male, lower socioeconomic level, not having statutory health insurance, not being in a relationship, living in western Germany and an urban area, and having insufficient social support. Comparing immigrants to non-immigrants, regular dental exams are around 36% less common among immigrants. |
| Calvasina, et al. (2016) | Canada | Questionnaire | No. 101
Age: >18 |
Examining the link between oral health literacy (OHL) and oral health care among Brazilian immigrants in Toronto, Ontario, Canada. | The majority of the sample (83.1%) had enough OHL. Lack of recent dental visits, not using a dentist as a key source of dental information, and not taking part in joint decisions about dental treatment were all linked to insufficient or minimal OHL. Two measures of inadequate oral care involvement were also linked to poor average annual family income. |
| Chen, et al. (2014) | Taiwan | Questionnaire | Νο. 590
Age: >18 |
Assessing the oral health practices of urban mothers and their children according to native versus immigrant status. | Compared to native mothers, immigrant mothers exhibited lower levels of caries knowledge and attitudes. Immigrant women were less likely than native mothers to floss, use toothpaste, visit the dentist within the previous two years, and take their children in for routine dental examinations, although they were more likely to abstain from sugary beverages. |
| Cruz, et al. (2020) | Spain | Questionnaire | No. 4568
Age: 3-14 |
Examine the socioeconomic and demographic factors related with dental problems and irregular utilization of dental services, as well as the prevalence of dental problems and the use of dental services in the Spanish-speaking and immigrant children’s population. | Compared to children of immigrants, Spanish-speaking children had a lower frequency of gingivitis (9.29%). The annual check-up was the most popular justification for visiting the dentist (Hispanics: 65.05%; immigrants: 54.94%). From age 7, there was a lower likelihood of non-regular use of dental services in both groups, albeit this probability increased with lower social status. Children from Spain who resided in cities with a population more than 10,000 had a lower risk of developing dental issues, whereas children older than 7 and those from lower socioeconomic classes had a higher likelihood. |
| Delgado-Angulo, et al. (2018) | UK | Questionnaire | No. 1910
Age: >18 |
Assessing the interaction between ethnicity, immigration status and dental caries among adults in East London. | While each Asian and black immigrant group had a lower DMFT than UK-born individuals of the same ethnic group, white immigrants had a higher DMFT* than people who were born in the UK. Age at arrival and length of residency were factors that were positively related to DMFT among persons who were foreign-born. |
| Ghiabi, et al (2014) | Canada | Interviews and clinical examination of the teeth | No. 86
Age: >18 |
A cohort of immigrants and refugees in Nova Scotia, Canada, underwent oral health reporting. | 85% of refugees and more than half (53%) of immigrants both had dental caries. The majority (73% of immigrants, 85% of refugees) had moderate to severe periodontitis, while 89% of immigrants and 98% of refugees, respectively, had moderate to severe gingivitis. But 64% of immigrants and 49% of refugees stated that they had good, very good, or outstanding dental health, and the majority claimed they didn’t require periodontal therapy or fillings. The study sample had better oral hygiene than the national norm, and there was a startling difference between self-reported and clinically determined dental care needs. |
| Kavathe,, et al. (2018) | USA | Assessment of local needs and resources | No. 169
Age: >18 |
Understanding how UNITED SIKHS developed its capacity to oversee participatory oral health projects by participating in community-based participatory research (CBPR) efforts and collecting local data. This helped the organization identify oral health as a priority need. | Fewer than half of the Sikh participants (43.0%) claimed they had never had an annual dental checkup, and only half (50.0%) of those who had said it had occurred within the previous year. Following a clinical evaluation, 58.2% of adult Sikhs were found to have dental caries. |
| Keboa, et al. (2019) | Canada | Interviews | No 25
Age: >18 |
Understanding how immigrants experience dental care and what they think may be done to increase access to dental care. | Participants’ dental care experiences included expensive charges, lengthy wait times, excellent care, close proximity to dental facilities, and delayed appointments. The introduction of community dental clinics, lower prices, integrating dental treatment into public insurance, and a more comprehensive health care strategy have all been proposed as ways to increase access to dental care. |
| Kohlenbergera, et al. (2019) | Austria | Contemporary (Interdisciplinary) research | No. 515
Age: >18 |
Identifying service use and the obstacles that refugees encounter while trying to get medical care. | The findings indicate that, particularly for women and Afghan refugees, the self-rated health of refugees is lower than that of the indigenous population. Four out of ten women and two out of ten men refugees report having unmet health requirements, despite the fact that respondents typically express high satisfaction with the Austrian healthcare system. The most frequently mentioned obstacles are language, lack of understanding about doctors, schedule issues, and lengthy waiting lists. Refugees reported using hospital services somewhat frequently, with hospitalizations being more common than hospital stays. |
| Macy, et al. (2018) | USA | Questionnaire | No. 157
Age: >21 |
Researchingthe usefulness and relevance of theoretical aspects connected to the search for preventive dental treatment in a sample of adult Mexican American immigrants. | Intention to seek preventive dental care was correlated with attitude toward seeking preventive dental care and self-efficacy for seeking preventive dental treatment. Both the relationship between past behavior and desire to seek preventative dental care and the association between dental beliefs and intention to do otherwise were mediated by attitude and self-efficacy. |
| Mehra, et al. (2019) | Canada | Telephone interview, questionnaire | No. 4208
Age: >12 |
The incidence of dental health care usage among immigrants and the relationships between different sociodemographic, socioeconomic, and health-related variables. | 33% of immigrants claimed they had not gone to the dentist in the previous year, and 25% said they had only gone in an emergency. Being a recent immigrant, male, with hardly any education, coming from a low-income family, and not having dental insurance were the top risk factors for overuse of dental care. |
| Muñoz‑Pino, et al. (2018) | Spain | Interview, questionnaire | No. 8591
Age: >18 |
Comparative analysis of the working immigrant population’s utilization of oral health care and the factors that influence it with that of their Spanish-speaking counterparts | Independent of oral health, sociodemographic, and socioeconomic variables, male immigrants were more likely to seek dental services for a year or more. |
| Nguyen, et. (2017) | USA | Questionnaire | No. 140
Age: >18 |
Investigating how Vietnamese Americans’ adoption of Western preventative dental care services is related to Vietnamese beliefs and practices about oral health. | Participants who agreed with the statement, “Regular visits to the dentist can help avoid dental problems,” were more likely to seek medical health services and visit a dentist if their “gums were bleeding,” according to Spearman Rank correlation testing. Only 22.86% of participants, however, said they would go to the dentist if they had a toothache. Participants did not believe that seeking Western oral health for all dental health difficulties, despite the results showing a substantial correlation between the use of medical health care services and the assumption that dental appointments can avoid future dental health issues. Age, gender, years lived in the United States, degree of education, religion, and specific oral beliefs and practices of the Vietnam survey participants did not show any statistical significance. |
| Nicol, et al. (2014) | Australia | Interview | No. 44
Age: >18 |
By examining preschool refugee families’, knowledge of ECC and children’ oral health, (ii) experiences using dental services, and (iii) obstacles and motivators for achieving better oral health, the authors intend to provide a deeper understanding of the refugee experience in relation to early oral health. | Categories included the significant impact of parents’ prior experiences, including their beliefs about milk (baby) teeth, traditional feeding practices, and poverty; as a result, there was a lack of understanding of the significance of early oral health and early dental care caries; (ii) the burden of resettlement, including prioritization, parenting, learning new foods, and how to integrate into the community; and (iii) refugees’ challenges in accessing both information and services. |
| Riggs, et al. (2014) | Australia | Interview | No. 115
Age: >18 |
Exploring experiences of using dental services from the perspective of migrant mothers living in Melbourne, Australia | The first dental contact for both women and their children was typically for emergency care, despite the fact that it was understood that going to the dentist was crucial for encouraging oral health. Significant barriers to participation were noted as cost, waiting lists, and accessibility. Negative experiences were frequently brought on by problematic interpreter encounters, which were made worse by the idea that public healthcare was of poorer quality. |
| Rota, et al. (2019) | USA | Questionnaire | No. 266
Age: >18 |
Exploring Oral Health Practices, Beliefs, Dental Visits, and Related Factors of Albanian Adults Living in Milwaukee, Wisconsin | Age, the ability to speak English, the typical source of dental treatment, and the report of excellent or good oral health were linked to dental visits in the previous year. Adults in Albania reported visiting the dentist frequently, and those who could speak English well reported visiting the dentist less frequently. |
| Solyman & Schmidt-Westhausen (2018) | Germany | Questionnaire | No. 386
Age >18 |
Assessing the oral health of recently arrived refugees in Germany and examining at their behaviors, attitudes, and knowledge about oral hygiene. | Women had considerably fewer missing teeth than males did, and the DMFT score was significantly correlated with age and education. The majority of participants had excellent attitudes and levels of knowledge about oral hygiene. |
| Xhihani, et al. (2017) | USA | Questionnaire | No. 211
Age: >18 |
Understanding the attitudes, habits, and beliefs of Albanian immigrants in the US about oral health. | According to the findings, a large percentage of respondents (68%) reported using dental services in the previous year. Despite the fact that 25% of participants claimed that their parents and grandparents had used folk medicines, 88% of participants claimed that the usage of folk remedies had no influence on their choice to seek out dental care from a professional. The notion that maintaining natural teeth is important was negatively connected to age, with older respondents being less likely to concur with the former statement. |
Σημείωση: *DMFT = decayed, missing and filled teeth
DISCUSSION
The study by Kohlenberger et al (2019) offers evidence on (1) refugees’ subjective well-being, (2) their access to and barriers to healthcare use, and (3) their impression of healthcare provision in Austria, one of the nations most impacted by the European refugee crisis. The Refugee Health and Inclusion Study (ReHIS), a cross-sectional survey of about 500 Syrian, Iraqi, and Afghan refugees, provided the core data on which it was based. The findings indicate that, particularly for women and Afghan refugees, the self-rated health of refugees is lower than that of the indigenous population. Four out of ten women and two out of ten men refugees report having unmet health requirements, despite the fact that respondents typically express high satisfaction with the Austrian healthcare system. The most frequently mentioned obstacles are language, lack of understanding about doctors, schedule issues, and lengthy waiting lists. Although the expense of care was not frequently considered to be a deterrent, refugees tend to consult dentists far less frequently than Austrians do. This is especially true of specialized medical services, which are frequently co-paid. Refugees reported using hospital services somewhat frequently, with hospitalizations occurring more frequently than hospital stays. (Kohlenberger et al., 2019).
Nguyen et al.’s (2017) study looked into Vietnamese oral health behaviors and beliefs and how they relate to Vietnamese Americans’ adoption of Western preventive dental care services. This study employed an exploratory cross-sectional survey design with a convenience sample of 140 people (n = 140). Participants responded to 28-question surveys delivered in paper form.Participants who agreed with the statement “Regular visits to the dentist can help avoid dental issues” were more likely to use medical services (p <0.05) and to visit a dentist if “gums were bleeding” (p <0.05), according to Spearman Rank correlation tests. Only 22.86% of participants, however, said they would go to the dentist if they had a toothache. Participants did not believe that pursuing Western oral health practices for all dental health difficulties, despite the findings revealing a substantial correlation between the usage of medical health care services and the assumption that dental visits can avoid future dental health issues. Age, gender, years spent in the country, native language, degree of education, religion, and specific oral beliefs and behaviors of individuals did not show any statistically significant correlations. (Nguyen et al., 2017).
The study by Solyman and Schmidt-Westhausen (2018) aimed to ascertain the oral health status of recently arrived migrants in Germany and explore their knowledge, attitudes, and oral hygiene behaviors. All participants (n = 386) were adults between the ages of 18 and 60 who were from Syria or Iraq and had registered as refugees in Germany during the previous year. An Arabic-language questionnaire was used to conduct the survey.Of the participants, 87 patients, or 5%, had untreated caries. The majority of participants had excellent attitudes and levels of knowledge about oral hygiene. However, the results revealed a discrepancy between their knowledge and practice. According to the data, newly arrived refugees in Germany had a significant frequency of untreated caries and poor dental hygiene. The study suggests emphasizing motivation in oral health promotion programs among refugees and giving them sufficient instructions on how to get oral healthcare in the host nation, ideally in their original language.(Solyman & Schmidt-Westhausen, 2018).
According to Xhihani et al. (2017) research, Albanians have a very high frequency of oral disease. Using a purposive sample (n = 211) of adult Albanian immigrants, descriptive research was conducted. A questionnaire was made available in both English and Albanian, with a 66 percent response rate. According to the findings, a large percentage of respondents (68%) reported using dental services in the previous year. Despite the fact that 25% of participants stated their parents and grandparents had utilized conventional treatments, 88% of them stated this had no bearing on their decision to seek out dental care from a professional.The value of maintaining natural teeth was inversely correlated with age because older respondents were less likely to concur with the former statement. It was more common for older responders to agree that bleeding gums were usual. The majority of Albanian immigrants studied did not have poor oral health care access or utilization as a contributing factor. Increased oral health awareness and potential improvements to the population’s poor oral health status could result from a focus on delivering age-appropriate behavioral techniques and oral health education. (Xhihani et al., 2017).
Muoz-Pino et al. (2018) compared the working immigrant population to their Spanish counterparts in order to examine the utilization of oral health services and associated factors. Using logistic regression, the relationship between the usage of oral health services and immigration status was evaluated.Independent of oral health, sociodemographic, and socioeconomic variables, male immigrants were more likely to use oral health services (aOR 1.63, 95% CI 1.26-2.02). After accounting for the same covariates, the higher likelihood that immigrant women would use oral health services dropped (aOR 1.15, 95% CI 0.91-1.45). Although there is a persisting discrepancy in the use of oral health services among immigrant men, occupational socioeconomic status and educational level may better explain the high prevalence of oral health service usage among immigrant women. (Muñoz-Pino et al., 2018).
In order to determine the association between ethnicity, immigrant status, and dental caries among adults in East London, Delgado-Angulo et al. (2018) conducted a study. 1910 adults (16-65) from 9 different ethnic groups who participated in an East London community health survey were the subjects of the data analysis. Participants filled out a questionnaire, and dentists with training conducted a clinical examination. The number of damaged, missing, and sealed teeth served as a measure of dental caries (DMFT).In negative binomial regression models that controlled for demographic, socioeconomic, and behavioral characteristics, the relationship between ethnicity and immigrant history and DMFT was examined. While each Asian and black immigrant group had a lower DMFT than UK-born individuals of the same ethnic group, white immigrants had a greater DMFT than people who were born in the UK. Age at arrival and length of residency were factors that were positively related to DMFT among persons who were foreign-born. Stronger differences between older and younger migrants with longer stays in the UK were discovered, indicating a significant interaction between the two factors. Adults born in the UK and those born abroad had considerable differences in their caries experiences, with significant variation amongst ethnic groups.(Delgado-Angulo et al., 2018).
By examining preschool refugee families’ understanding of children’s oral health, (ii) experiences of accessing dental services, and (iii) barriers and factors to achieving improved oral health, the study by Nicol et al. (2014) aimed to provide a deeper understanding of the refugee experience related to early oral health. Focus groups of newly settled refugee families and interviews with local refugee nurses both used qualitative technique. A bilingual community research associate was hired, and a community-based reference group was established. Eight focus groups with nine countries of origin and five interviews totaled 44 participants. Emerging themes included I the significant impact of parents’ past experiences, which included their beliefs about children’s teeth, traditional feeding practices, and poverty, and their lack of understanding of the significance of early oral health and early dental caries; (ii) the importance of resettlement, which included prioritization, parenting, learning new eating habits, and how to assimilate into the community; and (iii) refugees’ challenges in accessing both information and resources (Nicol et al., 2014).
Tambe Keboa et al.’s (2019) goal was to comprehend how immigrants in Montreal experienced dental care and what they thought should be done to increase access. They employed focused ethnography, which was inspired by a paradigm of public health for the delivery of dental treatment. An intentional sample of humanitarian migrants who sought or required dental care in Montreal was interviewed using the McGill Illness Narrative Adapted Interview (MINI). Each interview was taped for verbatim transcription and lasted 50–60 minutes. 25 participants—13 refugees and 12 asylum seekers—from ten different countries who had resided in Canada for a period ranging from one month to five years were spoken with. Participants’ dental care experiences included expensive charges, lengthy wait times, excellent care, close proximity to dental facilities, and delayed appointments. The introduction of community dental clinics, lower prices, integrating dental treatment into public insurance, and a more comprehensive health care strategy have all been proposed as ways to increase access to dental care. This study’s humanitarian migrants received insufficient dental care. The participants’ suggestions have a great chance to increase access to oral health care, and their lived experiences help to identify gaps in the provision of those services.(Keboa et al., 2019).
This study intends to examine migrant moms’ experiences accessing dental services while residing in Melbourne, Australia. It was decided to use a participatory research strategy with qualitative techniques. Participants included women from Pakistan, Lebanon, and Iraq. Focus groups and interviews that were semi-structured were held, and the data was then thematically analyzed. 115 women participated in focus groups (n = 11) and interviews (n = 7). The first dental contact for both women and their children was typically for emergency care, despite the fact that it was understood that going to the dentist was crucial for encouraging oral health. Significant barriers to participation were noted as cost, waiting lists, and accessibility. Negative experiences were frequently brought on by problematic interpreter encounters, which were made worse by the idea that public healthcare was of poorer quality. Immigrant women encounter severe challenges to receiving routine dental care, despite evidence of worse oral health. Reduced oral health disparities may result from refocusing such services to target accessibility and user experience for immigrant groups. (Riggs et al., 2014).
Mexican immigrants in the United States have poor dental health, according to Macy et al. (2018). The study’s goal was to examine the usefulness of putting theoretical considerations connected to seeking out preventive dental treatment in the sample of Mexican American adults. Data were gathered from a cross-sectional survey of 157 people of Mexican descent, 64% of whom were female and had an average age of 34 plus 11 years. Researchers tested for parameters linked with intention to seek preventive dental care using structural equation modelling, with the Integrated Behavior Prediction Model serving as the guiding framework. Intention to seek preventive dental care was correlated with attitude toward seeking preventive dental care (estimate= 0.37, p <.0001) and self-efficacy for seeking preventive dental care (estimate= 0.68, p <.0001). The relationship between prior behavior and intention to seek preventive dental treatment was mediated by efficacy, while the relationship between dental beliefs and desire to accomplish this was mediated by attitude and self-efficacy. These results imply that interventions to promote preventive dental care seeking among Mexican Americans should concentrate on modifying preventive dental care attitudes and elevating preventive dental care seeking self-efficacy. The results also support the use of treatments to change people’s perceptions about dentistry.(Macy et al., 2018).
The study by Calvasina et al. (2016) aimed to determine whether oral health literacy (OHL) and involvement in oral health care among Brazilian immigrants in Toronto, Ontario, Canada, were related. The study used a convenience sample of 101 Brazilian immigrants with a cross-sectional design. Descriptive statistics and logistic regression modelling were used to analyze the data. The majority of the sample (83.1%) had enough OHL. In multivariate logistic regressions controlling for covariates, low/marginal OHL was linked to not visiting the dentist in the previous year (OR = 3.61, p = 0.04), not having a dentist as the primary source of dental information (OR = 5.55, p <0.01), and not taking part in shared dental treatment decision making (OR = 1.06, p = 0.05, OHL as a continuous variable).A low average annual family income was linked to two signs of poor oral care involvement (ie, not visiting a dentist in the previous year and not having a dentist as a regular source of dental information). In a sample of Brazilian immigrants, low OHL was linked to reduced system participation and impediments to utilizing dental services. (Calvasina et al., 2016).
The study by Kavathe et al. (2018) aimed to understand how UNITED SIKHS identified oral health as a priority need by participating in community-based participatory research (CBPR) efforts and data gathering, consequently enhancing their capacity to lead participatory oral health projects. The collaborative implementation of a CBPR project to prevent diabetes in the Asian Indian Sikh community served as the basis for the partnership between UNITED SIKHS and the NYU Prevention Center (PRC).A community alliance made up of religious leaders, medical professionals, journalists, and academics and students at the NYU College of Dentistry was another project partner (NYU Dentistry). To better understand the health requirements of the Sikh community, a survey on community needs and resources was created and carried out in 2010. Less than half of the Sikh participants (43%) indicated they had never had a dental exam, and only half (50%) of those who had stated that they had within the last year. After a clinical evaluation, 58.2% of Sikh adults were found to have untreated dental caries. The gathering and evaluation of regional data prompted UNITED SIKHS to create fresh priorities in light of the results. To lead a project that created, put into practice, assessed, and disseminated a culturally appropriate oral health and healthy living education program for the Asian Indian Sikh community, UNITED SIKHS applied for and obtained outside financing.(Kavathe et al., 2018).
In their 2018 study, Pullen, Perry, and Maupome examined the impact of individual and egocentric traits on two measures of oral health service consumption using data from 332 Mexican immigrants. Findings show that the usage of oral health services is positively correlated with network size, network dental service use, and the frequency with which immigrants discuss network links. The probability of using these services is, on the other hand, lower when embedded in networks where egos participate in dental concerns and have poor levels of dental health knowledge. This study is one of the first to investigate at how network factors affect oral health behaviors in this underprivileged community using network data and methodology. (Pullen et al., 2018).
In Nova Scotia, Canada, 45 recent immigrants and 41 recent Bhutanese refugees, ages 18 to 67, underwent an oral health questionnaire and a clinical oral examination. 85% of refugees and more than 50% of immigrants both had untreated dental caries. The majority (73% of immigrants, 85% of refugees) had moderate to severe periodontitis, while 89% of immigrants and 98% of refugees, respectively, had moderate to severe gingivitis. But 64% of immigrants and 49% of refugees stated that they had good, very good, or outstanding dental health, and the majority claimed they didn’t require periodontal therapy or fillings. The study population had greater rates of oral disease than the national average, and there was a startling difference between self-reported and clinically determined dental care needs. (Ghiabi et al., 2014).
The study conducted by Brzoska et al. (2017) aimed to investigate the significance of oral health among immigrants and non-immigrants living in Germany. Utilizing information on preventative oral health behaviors from n = 41,220 people, 15% of whom are immigrants, cross-sectional national health surveys were used. The conceptual basis of the study is Andersen’s Behavioral Model of Health Service Use. To explore the role of various predisposing and predisposing factors, multiple logistic regression models were used. In order to determine whether the determinants differ for immigrants and non-immigrants, interaction terms were introduced. Comparing immigrants to non-immigrants, regular dental exams are around 36% less common among immigrants. The influence of demographic, social, behavioral, and health-related factors help to explain some of the disparities. Lower odds of using routine dental exams were connected with younger age, being a guy, having a lower socioeconomic situation, not having legal health insurance, not being in a relationship, residing in western Germany, living in an urban area, and having less social support. Effects of interactions between age and the type of health insurance could be observed. The study reveals a variety of initiating and predisposing factors, some of which vary between immigrants and non-immigrants, that are connected to the usage of dental examinations in the population in Germany. For younger ages, the inequalities are particularly noticeable. This is in contrast to other preventative services’ findings, which show that older immigrants are typically more disadvantageous.(Brzoska et al., 2017).
Based on information from the 2017 National Health Survey in Spain, the study by de la Cruz and Cebrino (2020) set out to determine the prevalence of dental problems and the use of dental services in the population of children from Spain and immigrants, as well as to determine the type of treatment and analyze the socioeconomic and demographic variables related to dental problems and the non-regular use of dental services. The sample included 4568 children between the ages of 3 and 14.Using logistic regression models, the relationship between dental service use and dental issues was examined in connection to socioeconomic and demographic factors. Children in Spain had a caries prevalence of 9.29% compared to immigrants’ 18.58% (p <0.001). Checkups were the most frequent cause for dental appointments (Hispanics: 65.05%; immigrants: 54.94%). From age 7, there was a lower likelihood of non-regular use of dental services in both groups, albeit this probability increased with lower social status. Children from Spain who resided in cities with a population more than 10,000 had a lower risk of developing dental issues, whereas children older than 7 and those from lower socioeconomic classes had a higher likelihood.(de la Cruz & Cebrino, 2020).
In order to understand the prevalence of dental health care usage among Ontario’s immigrant community and how different sociodemographic, socioeconomic, and health-related factors are associated with it, Mehra et al. (2019) conducted a study. On a total of 4208 immigrants from Ontario, the analysis was done. The two factors of not visiting the dentist in the previous year and/or visiting only in an emergency were used to define underutilization of dental care.To examine relationships between the two outcomes and sociodemographic, socioeconomic, and health-related factors, multivariate logistic regression was used. 33% of immigrants stated that they had not gone to the dentist in the previous year, and 25% said they had only gone in an emergency. Being an immigrant, male, with low education, low family income, and not having dental insurance were the top risk factors for overuse of dental care. This study is the first to show how immigrants in Ontario use oral care services. Given that a high proportion of immigrants in Ontario underuse dental treatment, education and outreach initiatives that enlighten newcomers about preventative dental care may enhance general oral health. (Mehra et al., 2019).
Rota et al.’s (2019) research examined into the dental appointments, practices, and related characteristics of Albanian people living in Milwaukee, Wisconsin. Data on dental visits, oral health behaviors, beliefs, and sociodemographic details were gathered using questionnaires. 266 persons in total were recruited; 54% of them were men, 56% had lived in the US for 10 years or more, 95% evaluated their dental health as excellent or good, and 87% said they had seen the dentist within the previous year. Age, English language proficiency, regular dental care provider, and reporting excellent/good oral health were all linked to dental visits in the previous year. Adults in Albania reported visiting the dentist frequently in the previous year, and those who could not read or write in English were less likely to do so. (Rota et al., 2019).
Chen et al. (2014) examined immigrant-native variations in mothers’ and their children’ oral health behaviors. A cross-sectional study was carried out to gather information from moms in a Taiwanese urban region. The self-report questionnaires were filled out by 440 native moms and 150 immigrant mothers in total. Racial variations in oral health practices were examined using logistic regression models. Only 13.5% of migrant mothers routinely visited a dentist, although 37% of them flossed and 25% used fluoridated toothpaste. Fewer than 40% of immigrant mothers brush their kids’ teeth before they turn a year old, 45% change the kid’s toothbrush after three months, and just 50% of mothers frequently take their kids to the dentist. Compared to native moms, immigrant mothers exhibited lower levels of knowledge and attitudes towards caries (p<0.001). Immigrant women were less likely than mothers who were native-born to floss, use fluoride toothpaste, see the dentist within the previous two years, or take their kids in for routine dental exams, although they were more likely to avoid sweetened soft beverages. Immigrant moms had lower levels of oral health knowledge, attitudes, and behaviors related to dental caries than native mothers. Findings imply that cross-cultural caries prevention initiatives should be created for these immigrant minorities of the children in order to reduce immigrant-native oral care inequities. (Chen et al., 2014).
CONCLUSION
Migration is a social determinant of health, including oral health(Sano & Abada, 2019). Comparing immigrants to their native-born counterparts, higher incidence of dental disease and underuse of dental care have been observed(Bedi & Elton, 1991; Wang, 1996), especially among those who had lived in the host country for less than 10 years(Akresh, 2009; Cruz et al., 2010). Additionally, immigrants receive fewer preventative services and more treatments compared to native-born children, who frequently visit dentists for preventive care(Newbold & Patel, 2006). As a result, there are serious public health concerns regarding the disparities in oral health among immigrants that should not be ignored.
Integration is thought to be the most desired technique for immigrants’ adaptation during their acculturation process because acculturation strategies depend on immigrants’ adaptation; marginalization, on the other hand, has largely negative effects(Berry et al., 2006). Additionally, immigrant adaptation is a lifelong process that results in various coping mechanisms in individuals. Even the same individual may adopt various coping mechanisms at different stages of acculturation(Yu & Wang, 2011).
Community leaders with a background in health promotion can help immigrant and refugee families by providing dental education. These people are able to communicate with new parents, raise their understanding of preventative care and oral health, and make it easier for their children to get access to dental treatment.
Immigrants’ and ethnic minorities’ oral health is significantly impacted by changes in social life after immigration. In order to determine the relationships between social support and oral health outcomes in this population, this study thoroughly evaluated the literature and discovered a variety of relationships. Immigrants and members of ethnic minorities who receive social support from their immediate community (such as family and friends) or from society at large use dental services more frequently and have better oral health overall, including lower levels of caries and periodontal disease.Social support also improved self-rated dental health and quality of life connected to oral health. People from ethnic minorities and immigrants who had strong social ties also understood more about oral health and dental care.
Funding details: No funding was received.
Disclosure statement: The authors report there are no competing interests to declare.
REFERENCES
- Adibi, S., Li, M., Salazar, N., Seferovic, D., Kookal, K., Holland, J. N., Walji, M., & Farach-Carson, M. C. (2020). Medical and Dental Electronic Health Record Reporting Discrepancies in Integrated Patient Care. JDR Clinical and Translational Research, 5(3), 278–283. https://doi.org/10.1177/2380084419879387
- Akresh, I. R. (2009). Health service utilization among immigrants to the united states. Population Research and Policy Review, 28(6), 795–815. https://doi.org/10.1007/s11113-009-9129-6
- Batra, M., Gupta, S., & Erbas, B. (2019). Oral health beliefs, attitudes, and practices of south Asian migrants: A systematic review. International Journal of Environmental Research and Public Health, 16(11). https://doi.org/10.3390/ijerph16111952
- Bedi, R., & Elton, R. A. (1991). Dental caries experience and oral cleanliness of Asian and white Caucasian children aged 5 and 6 years attending primary schools in Glasgow and Trafford, UK. Community Dental Health, 8(1), 17–23. https://pubmed.ncbi.nlm.nih.gov/2049651/
- Berry, J. W., Phinney, J. S., Sam, D. L., & Vedder, P. (2006). Immigrant youth: Acculturation, identity, and adaptation. Applied Psychology, 55(3), 303–332. https://doi.org/10.1111/j.1464-0597.2006.00256.x
- Brzoska, P., Erdsiek, F., & Waury, D. (2017). Enabling and predisposing factors for the utilization of preventive dental health care in migrants and non-migrants in Germany. Frontiers in Public Health, 5(AUG). https://doi.org/10.3389/fpubh.2017.00201
- Calvasina, P., Lawrence, H. P., Hoffman-Goetz, L., & Norman, C. D. (2016). Brazilian immigrants’ oral health literacy and participation in oral health care in Canada. BMC Oral Health, 16(1), 1–7. https://doi.org/10.1186/s12903-016-0176-1
- Chen, C. C., Chiou, S. J., Ting, C. C., Lin, Y. C., Hsu, C. C., Chen, F. L., Lee, C. H., Chen, T., Chang, C. S., Lin, Y. Y., & Huang, H. L. (2014). Immigrant-native differences in caries-related knowledge, attitude, and oral health behaviors: A cross-sectional study in Taiwan. BMC Oral Health, 14(1), 1–9. https://doi.org/10.1186/1472-6831-14-3
- Cruz, G. D., Chen, Y., Salazar, C. R., Karloopia, R., & LeGeros, R. Z. (2010). Determinants of oral health care utilization among diverse groups of immigrants in New York City. Journal of the American Dental Association, 141(7), 871–878. https://doi.org/10.14219/jada.archive.2010.0286
- Dahlan, R., Badri, P., Saltaji, H., & Amin, M. (2019). Impact of acculturation on oral health among immigrants and ethnic minorities: A systematic review. PLoS ONE, 14(2). https://doi.org/10.1371/journal.pone.0212891
- de la Cruz, S. P., & Cebrino, J. (2020). Oral health problems and utilization of dental services among spanish and immigrant children and adolescents. International Journal of Environmental Research and Public Health, 17(3). https://doi.org/10.3390/ijerph17030738
- Delgado-Angulo, E. K., Marcenes, W., Harding, S., & Bernabé, E. (2018). Ethnicity, migration status and dental caries experience among adults in East London. Community Dentistry and Oral Epidemiology, 46(4), 392–399. https://doi.org/10.1111/cdoe.12381
- Farmaki, A., & Christou, P. (2019). Refugee migration and service industries: advancing the research agenda. Service Industries Journal, 39(9–10), 668–683. https://doi.org/10.1080/02642069.2018.1435643
- Ferreira, M. C., Dias-Pereira, A. C., Branco-de-Almeida, L. S., Martins, C. C., & Paiva, S. M. (2017). Impact of periodontal disease on quality of life: a systematic review. In Journal of Periodontal Research (Vol. 52, Issue 4, pp. 651–665). https://doi.org/10.1111/jre.12436
- Gao, X. L. (2011). A review on the oral health impacts of acculturation. In Journal of Immigrant and Minority Health (Vol. 13, Issue 2, pp. 202–213). https://doi.org/10.1007/s10903-010-9414-9
- Ghiabi, E., Matthews, D. C., & Brillant, M. S. (2014). The oral health status of recent immigrants and refugees in nova Scotia, Canada. Journal of Immigrant and Minority Health, 16(1), 95–101. https://doi.org/10.1007/s10903-013-9785-9
- Hilton, I. V., Stephen, S., Barker, J. C., & Weintraub, J. A. (2007). Cultural factors and children’s oral health care: A qualitative study of carers of young children. Community Dentistry and Oral Epidemiology, 35(6), 429–438. https://doi.org/10.1111/j.1600-0528.2006.00356.x
- Hunt, R. J., Slade, G. D., & Strauss, R. P. (1995). Differences between Racial Groups in the Impact of Oral Disorders among Older Adults in North Carolina. Journal of Public Health Dentistry, 55(4), 205–209. https://doi.org/10.1111/j.1752-7325.1995.tb02371.x
- Jin, L. J., Lamster, I. B., Greenspan, J. S., Pitts, N. B., Scully, C., & Warnakulasuriya, S. (2016). Global burden of oral diseases: emerging concepts, management and interplay with systemic health. In Oral Diseases (Vol. 22, Issue 7, pp. 609–619). https://doi.org/10.1111/odi.12428
- Kavathe, R., Islam, N., Zanowiak, J., Wyatt, L., Singh, H., & Northridge, M. E. (2018). Building capacity in the sikh asian indian community to lead participatory oral health projects. Progress in Community Health Partnerships: Research, Education, and Action, 12(1), 3–14. https://doi.org/10.1353/cpr.2018.0001
- Keboa, M. T., Hovey, R., Nicolau, B., Esfandiari, S., Carnevale, F., & Macdonald, M. E. (2019). Oral healthcare experiences of humanitarian migrants in Montreal, Canada. Canadian Journal of Public Health, 110(4), 453–461. https://doi.org/10.17269/s41997-019-00193-5
- Klinge, B., & Norlund, A. (2005). A socio-economic perspective on periodontal diseases: A systematic review. Journal of Clinical Periodontology, 32(SUPPL. 6), 314–325. https://doi.org/10.1111/j.1600-051X.2005.00801.x
- Kohlenberger, J., Buber-Ennser, I., Rengs, B., Leitner, S., & Landesmann, M. (2019). Barriers to health care access and service utilization of refugees in Austria: Evidence from a cross-sectional survey. Health Policy, 123(9), 833–839. https://doi.org/10.1016/j.healthpol.2019.01.014
- Leung, G., & Stanner, S. (2011). Diets of minority ethnic groups in the UK: Influence on chronic disease risk and implications for prevention. Nutrition Bulletin, 36(2), 161–198. https://doi.org/10.1111/j.1467-3010.2011.01889.x
- Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P. A., Clarke, M., Devereaux, P. J., Kleijnen, J., & Moher, D. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ (Clinical Research Ed.), 339. https://doi.org/10.1136/bmj.b2700
- Macy, J. T., Moser, E. A. S., Hirsh, A. T., Monahan, P. O., Eckert, G. J., & Maupomé, G. (2018). Factors associated with seeking preventive dental care: An integrative model exploration of behaviors in Mexican immigrants in Midwest America. BMC Oral Health, 18(1), 1–6. https://doi.org/10.1186/s12903-018-0502-x
- Mehra, V. M., Costanian, C., Khanna, S., & Tamim, H. (2019). Dental care use by immigrant Canadians in Ontario: A cross-sectional analysis of the 2014 Canadian Community Health Survey (CCHS). BMC Oral Health, 19(1), 1–9. https://doi.org/10.1186/s12903-019-0773-x
- Milnes, A. R. (1996). Description and epidemiology of nursing caries. Journal of Public Health Dentistry, 56(1), 38–50. https://doi.org/10.1111/j.1752-7325.1996.tb02394.x
- Muñoz-Pino, N., Vives-Cases, C., Agudelo-Suárez, A. A., & Ronda-Pérez, E. (2018). Comparing Oral Health Services Use in the Spanish and Immigrant Working Population. Journal of Immigrant and Minority Health, 20(4), 809–815. https://doi.org/10.1007/s10903-017-0630-4
- Newbold, K. B., & Patel, A. (2006). Use of dental services by immigrant Canadians. In Journal of the Canadian Dental Association (Vol. 72, Issue 2). https://pubmed.ncbi.nlm.nih.gov/16545174/
- Nguyen, K. Y. T., Smallidge, D. L., Boyd, L. D., & Rainchuso, L. (2017). Vietnamese Oral Health Beliefs and Practices: Impact on the Utilization of Western Preventive Oral Health Care. Journal of Dental Hygiene : JDH, 91(1), 49–56. https://jdh.adha.org/content/91/1/49
- Nicol, P., Al-Hanbali, A., King, N., Slack-Smith, L., & Cherian, S. (2014). Informing a culturally appropriate approach to oral health and dental care for pre-school refugee children: A community participatory study. BMC Oral Health, 14(1), 69. https://doi.org/10.1186/1472-6831-14-69
- Organization World Health. (2015). Guideline: Sugars intake for adults and children. World Health Organization, 57(6), 1716–1722. https://www.who.int/publications/i/item/9789241549028?fbclid=IwAR2JITq5jdX1PSq1LC7BE_5vilXlfOOQAvK_MfwHv_cXYcNFAo2S2DISrkY
- Patel, R. (2017). The State of Oral Health in Europe: Better Oral Health European Platform. 2012. In Community Dental Health (Vol. 29, Issue 2).
- Pelizza, A. (2020). Processing Alterity, Enacting Europe: Migrant Registration and Identification as Co-construction of Individuals and Polities. Science Technology and Human Values, 45(2), 262–288. https://doi.org/10.1177/0162243919827927
- Petersen, P. E. (2003). The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century – The approach of the WHO Global Oral Health Programme. Community Dentistry and Oral Epidemiology, 31(SUPPL. 1), 3–24. https://doi.org/10.1046/j..2003.com122.x
- Petersen, P. E., Bourgeois, D., Ogawa, H., Estupinan-Day, S., & Ndiaye, C. (2005). The global burden of oral diseases and risks to oral health. In Bulletin of the World Health Organization (Vol. 83, Issue 9, pp. 661–669). https://doi.org//S0042-96862005000900011
- Pullen, E., Perry, B. L., & Maupome, G. (2018). “Does this Look Infected to You?” Social Network Predictors of Dental Help-Seeking Among Mexican Immigrants. Journal of Immigrant and Minority Health, 20(2), 399–409. https://doi.org/10.1007/s10903-017-0572-x
- Reher, D., & Requena, M. (2009). The national immigrant survey of Spain: A new data source for migration studies in Europe. Demographic Research, 20, 253–278. https://doi.org/10.4054/DemRes.2009.20.12
- Riedy, C. A., Weinstein, P., Milgrom, P., & Bruss, M. (2001). An ethnographic study for understanding children’s oral health in a multicultural community. International Dental Journal, 51(4), 305–312. https://doi.org/10.1002/j.1875-595X.2001.tb00843.x
- Riggs, E., Gussy, M., Gibbs, L., Van Gemert, C., Waters, E., & Kilpatrick, N. (2014). Hard to reach communities or hard to access services? Migrant mothers’ experiences of dental services. Australian Dental Journal, 59(2), 201–207. https://doi.org/10.1111/adj.12171
- Rota, K., Spanbauer, C., Szabo, A., & Okunseri, C. E. (2019). Oral Health Practices, Beliefs and Dental Service Utilization of Albanian Immigrants in Milwaukee, Wisconsin: A Pilot Study. Journal of Immigrant and Minority Health, 21(2), 315–323. https://doi.org/10.1007/s10903-018-0738-1
- Sano, Y., & Abada, T. (2019). Immigration as a Social Determinant of Oral Health: Does the “Healthy Immigrant Effect” Extend to Self-rated Oral Health in Ontario, Canada? Canadian Ethnic Studies, 51(1), 135–156. https://doi.org/10.1353/ces.2019.0005
- Satcher, D. (2017). Revisiting oral health in America: A report of the surgeon general. In American Journal of Public Health (Vol. 107, pp. S32–S33). https://doi.org/10.2105/AJPH.2017.303687
- Scholten, P., Entzinger, H., & Penninx, R. (2015). Research-Policy Dialogues on Migrant Integration in Europe: A Conceptual Framework and Key Questions. In IMISCOE Research Series (pp. 1–16). https://doi.org/10.1007/978-3-319-16256-0_1
- Shevchenko, P. E. (2020). The effect of using the terms “refugee” and “migrant” as synonyms in the online versions of le monde and le temps newspapers in 2015-2016. Vestnik Moskovskogo Universiteta. Seriya 10. Zhurnalistika, 2020(1), 102–128. https://doi.org/10.30547/vestnik.journ.1.2020.102128
- Skeie, M. S., Riordan, P. J., Klock, K. S., & Espelid, I. (2006). Parental risk attitudes and caries-related behaviours among immigrant and western native children in Oslo. Community Dentistry and Oral Epidemiology, 34(2), 103–113. https://doi.org/10.1111/j.1600-0528.2006.00256.x
- Solyman, M., & Schmidt-Westhausen, A. M. (2018). Oral health status among newly arrived refugees in Germany: A cross-sectional study. BMC Oral Health, 18(1), 1–9. https://doi.org/10.1186/s12903-018-0600-9
- Steele, J., Shen, J., Tsakos, G., Fuller, E., Morris, S., Watt, R., Guarnizo-Herreño, C., & Wildman, J. (2015). The interplay between socioeconomic inequalities and clinical oral health. Journal of Dental Research, 94(1), 19–26. https://doi.org/10.1177/0022034514553978
- Tezal, M., Grossi, S. G., Ho, A. W., & Genco, R. J. (2004). Alcohol consumption and periodontal disease: The third national health and nutrition examination survey. Journal of Clinical Periodontology, 31(7), 484–488. https://doi.org/10.1111/j.1600-051X.2004.00503.x
- van der Putten, G. J., Vanobbergen, J., De Visschere, L., Schols, J., & de Baat, C. (2009). Association of some specific nutrient deficiencies with periodontal disease in elderly people: A systematic literature review. In Nutrition (Vol. 25, Issues 7–8, pp. 717–722). Nutrition. https://doi.org/10.1016/j.nut.2009.01.012
- Vartanian, L. R., Schwartz, M. B., & Brownell, K. D. (2007). Effects of soft drink consumption on nutrition and health: A systematic review and meta-analysis. In American Journal of Public Health (Vol. 97, Issue 4, pp. 667–675). Am J Public Health. https://doi.org/10.2105/AJPH.2005.083782
- Wang, N. J. (1996). Dental caries and resources spent for dental care among immigrant children and adolescents in Norway. International Dental Journal, 46(2), 86–90. https://pubmed.ncbi.nlm.nih.gov/8930679/
- Watt, R., & Sheiham, A. (1999). Inequalities in oral health: a review of the evidence and recommendations for action. British Dental Journal, 187(1), 6–12. https://doi.org/10.1038/sj.bdj.4800191
- Wickramage, K., Vearey, J., Zwi, A. B., Robinson, C., & Knipper, M. (2018). Migration and health: A global public health research priority. BMC Public Health, 18(1). https://doi.org/10.1186/s12889-018-5932-5
- Xhihani, B., Rainchuso, L., Smallidge, D., & Dominick, C. (2017). Oral Health Beliefs, Attitudes, and Practices of Albanian Immigrants in the United States. Journal of Community Health, 42(2), 235–241. https://doi.org/10.1007/s10900-016-0248-9
- Yu, W., & Wang, S. (2011). An Investigation into the Acculturation Strategies Of Chinese Students in Germany. Intercultural Communication Studies, 20(2), 190–210. http://web.uri.edu/iaics/files/15WeihuaYuShuWang.pdf